stournsaeh / shutterstock.com
The data tell the story. Despite improvements in overall outcomes for common rheumatologic conditions, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), white patients fare better than minority patients, and sometimes substantially better. Even with new biologic therapies that have significantly altered the course of disease for patients with RA, outcomes for minorities lag behind those of whites. A 2013 study by Greenberg et al. showed that white patients with RA had significantly improved outcomes compared with minority patients. Using data collected from a large cohort of community-based rheumatology practices on patients treated between 2005 and 2007 and 2010 and 2012, the study found that disease activity levels and remission rates in whites were significantly better than in minorities during both time periods.1
For patients with lupus, data on outcomes, incidence and prevalence rates continue to show that non-whites bear the greater burden of this disease. Recent studies continue to show a higher incidence and prevalence rates of lupus in minorities compared with whites, with the highest prevalence rates in non-Hispanic black women.2-4 In addition, blacks have earlier onset of the disease and experience increased rates of renal disease and progression to end-stage renal disease (ESRD) compared with whites.4
These recent studies are just a sampling of data long established on the disparate outcomes seen between whites and minorities in rheumatology, and mirror what is well documented in other clinical areas. Just do a PubMed search with “racial disparities” as the search term, and thousands of studies come up documenting and discussing this issue across most, if not all, areas of healthcare.
Recognition of the range and depth of this problem across medicine was highlighted in a report published in 2002 by the Institutes of Health (IOH), titled “Unequal Treatment,” which focused national attention on racial and ethnic disparities in health and spurred the creation of an annual report published by the Agency for Healthcare Research and Quality (AHRQ) that reports on healthcare quality and disparities.5 Called the National Healthcare Quality and Disparities Report, it provides an annual update on quality of and access to healthcare. More recently, national efforts to reduce health disparities include the Department of Health and Human Services (HHS) Disparities Action Plan in 2011 and the expansion of insurance coverage under the Affordable Care Act.
Just do a PubMed search with ‘racial disparities’ as the search term, & thousands of studies come up.
You can find current data on these efforts and a good discussion of key questions and answers about health disparities at the Henry J Kaiser Family Foundation (KFF).6 Among the important issues addressed by the KFF is the complex and interrelated variables that contribute to health disparities, including social/environmental factors (e.g., poverty, education, proximity to care and neighborhood safety), health system (e.g., how healthcare is organized, financed and delivered), patient factors (e.g., health behaviors) and provider factors (e.g., bias and cultural/linguistic barriers to patient-provider communication).6
In this sampling of studies and resources devoted to addressing health disparities, we see how deeply entrenched these disparities are in the U.S. healthcare system, and the ongoing need to address not only what many see as a societal wrong but what is also an unsustainable extra cost to an already overburdened healthcare system. As noted in the KFF report, roughly 30% of total direct medical costs for minorities (i.e., blacks, native Americans, Hispanics and Asians) are excess costs caused by health inequities.6
Moving beyond study and rhetoric to action that can reduce and remove these racial disparities is becoming all the more imperative given the rapidly changing demographics of the U.S., which is becoming more racially and ethnically diverse. Currently, nearly four in 10 (38%) of persons living in the U.S. are people of color. By 2045, people of color are projected to comprise more than 50% of the population, with the largest growth in Hispanics.6
To contribute to the ongoing effort to help reduce racial health disparities, the ACR has undertaken a number of initiatives over the past several years.
Addressing Racial Disparities in Rheumatology

Dr. Lim
S. Sam Lim, MD, MPH, clinical director in the Division of Rheumatology at Emory University in Atlanta and the chair of a working group within the ACR assembled to advance health equity and eliminate health disparities in rheumatology, is particularly plugged into the issue of racial disparities in rheumatology. Looking at the issue broadly, he emphasizes that the factors that contribute to racial/ethnic health disparities in rheumatology are fundamentally the same as those found in other fields, including complex and interrelated biological, behavioral, provider, healthcare system, societal and environmental factors.
“In many of the complex, systemic conditions rheumatologists treat, most of these factors are amplified,” he says, citing as an example the “particularly profound” gender and racial disparities in SLE.
Saying he thinks rheumatologists “work hard every day to mitigate various factors that contribute to disparities in care and outcomes” and are taking tangible steps to reduce disparities, he nonetheless believes “many need and seek additional steps they can take and resources available to them, their staff and their patients.”
One such resource is a new initiative the ACR calls Uniting Collaborators for Innovation (UCOIN). The ACR developed UCOIN as a way for members to generate, design and implement projects or to assist in ongoing projects to advance the mission of the ACR. Members are encouraged to use UCOIN as a platform to submit ideas and work with other members to collectively solve problems affecting the practice of rheumatology and the care of patients.

Ms. McCalla
Recently, UCOIN was one of five programs awarded $10,000 by the American Society of Association Executives Foundation’s Innovation Grants Program in recognition of its innovative efforts. According to Dr. Lim, this was a particularly competitive round of applications, and validates what the ACR is doing as innovative and important.
According to Sheryl McCalla, UCOIN project director and the ACR vice president of collaborative initiatives, the initial phase of UCOIN is creating member-driven initiatives to eliminate racial and ethnic health disparities within rheumatology.
“We put out a call to see who would like to work with us on projects having to do with health disparities,” she says. Members were asked to submit letters of interest, and Ms. McCalla and her staff worked with selected members to develop and submit proposals to the funder by late March. Two projects were funded and began in July 2018.
The ACR is also working on proposals that address increasing the number of minorities who participate in clinical trials as well as increasing healthcare access. Both the lack of minority representation in clinical trials and barriers to healthcare access were identified by UCOIN organizers as potentially negatively affecting minority populations with rheumatologic conditions.
Building on Past Success
If the past is prologue, UCOIN should succeed. According to Ms. McCalla, UCOIN is an outgrowth of The Lupus Initiative (TLI) that was launched by the ACR in 2009, with funding from the Office of Minority Health, the Office of Women’s Health and the Surgeon General, to get members involved in reducing health disparities in lupus by developing educational resources on lupus.
“The idea of UCOIN is to broaden and build on what we’ve done in lupus,” she says, “and to use the process of UCOIN as a platform for innovation so our members can drive the thinking about how to tackle these issues across all of rheumatology.”
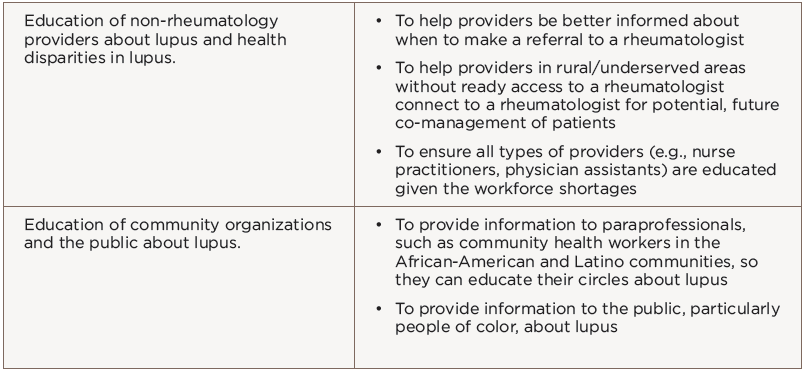
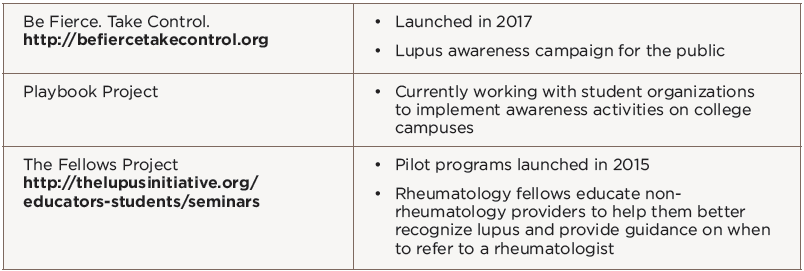
To date, TLI has produced a number of successful projects aimed at reducing disparities in lupus, most of which focus on education (see Table 1). Table 2 cites a few examples of specific educational programs offered through TLI.
Ms. McCalla emphasizes that success with these programs was not linear and required a learning curve marked by much trial and error. Among the lessons learned was the amount of agility required to allow members to complete their projects within short time frames. In addition, they learned collaboration across internal ACR departments and organizations external to the ACR is needed to develop projects with bold objectives with short time frames, and that members need innovative space to take calculated risks.
“The concept for UCOIN evolved from the desire to duplicate the conditions that allowed the success of TLI,” says Ms. McCalla, “and to leverage the lessons learned to enable the ACR to anticipate and manage challenges that will result from scaling up.”
If UCOIN follows the lessons of TLI, it should enjoy much success. Ms. McCalla underscores that the initial vision for TLI as a stand-alone, short-term experiment has blossomed into a national, well-respected health disparities program.
Because UCOIN is still in its infancy phase, Ms. McCalla encourages member input to help refine both the concept of UCOIN as well as the processes that support it. UCOIN will officially launch at the 2018 annual meeting.
Ms. McCalla urges members to keep an eye out for the launch at the annual meeting, as well as for information leading up to the annual meeting that will better inform them about the resources and opportunities available to them regarding UCOIN and how to access them.
For more information, contact Dr. Lim at [email protected] or Ms. McCalla at [email protected].
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
References
- Greenberg JD, Spruill TM, Shan Y, et al. Racial and ethnic disparities in disease activity in rheumatoid arthritis patients. Am J Med. 2013 Dec;126(12):1089–1098.
- Izmirly PM, Wan I, Sahl S, et al. The incidence and prevalence of systemic lupus erythematous: The Manhattan Lupus Surveillance Program. Arthritis Rheumatol. 2017 Oct;69(10):2006–2017.
- Dall’Era M, Cisternas MG, Snipes K, et al. The incidence and prevalence of systemic lupus erythematous: The California Lupus Surveillance Project. Arthritis Rheumatol. 2017 Oct;69(10):1996–2005.
- Somers EC, Marder W, Cagnoli P, et al. Population-based incidence and prevalence of systemic lupus erythematosus: The Michigan Lupus Epidemiology and Surveillance Program. Arthritis Rheumatol. 2014 Feb;66(2):369–378.
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. National Academies Press, 2003.
- Ubri P, Artiga S. (2016 Aug). Disparities in Health and Healthcare: Five Key Questions and Answers.