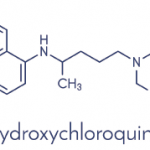
A total of 1,808 (37%) patients reported HCQ use, with a median duration of use of 3.1 years. The rate of new diabetes diagnoses was 5.2 per 1,000 patient-years in the HCQ group and 8.9 per 1,000 in the group not reporting HCQ use. The adjusted reduction in diabetes risk was 38% (95% CI, 8–58%). The multivariable adjusters were broad, including age, gender, race, education, duration of RA, HAQ-DI score, methotrexate, and prednisone use. Moreover, longer exposure was associated with greater risk reduction. (See Table 1, above.)
These results are very provocative and add to a small literature suggesting a hypoglycemic effect of HCQ.2,3 Before we accept these results as truth, the methodologic limitations of this study should be examined. This type of pharmaco-epidemiologic analysis is only as good as the characterization of exposure, definition of endpoint, and control for confounding. The authors have used semi-annual survey reports to assess the exposure. The validity of the patient report of medications and the assumptions regarding medication use between surveys are untested. However, typically, the expected misclassification of exposure biases findings toward the null, not away from the null as observed in this study.
The definition of diabetes is the weakest aspect of the study design. The authors require a patient report of diabetes or new use of a hypoglycemic medication. They state that use of a hypoglycemic agent in subsequent periods was used to “verify” diabetes for patients not reporting medication use at diabetes onset. But less than half of the patients on HCQ with new-onset diabetes reported subsequent use of a hypoglycemic agent. The authors suggest that this observation supports HCQ’s role as a hypoglycemic agent itself; however, I found the definition of diabetes confusing and the fact that so few patients required a specific medication for diabetes was implausible.
Finally, the study’s ability to control for potential confounders was not clear. Glucocorticoid use was assessed, but only represented as a dichotomous variable and not as a continuous cumulative or daily dosage. There was no information about the risk of diabetes associated with glucocorticoid use or any other covariate. It is possible that HCQ’s observed benefits work through a reduction in glucocorticoid cumulative dosage or a substation for another disease-modifying anti-rheumatic drug. Also, there was no information about a patient’s level of exercise or family history of diabetes, two potential confounders.
The authors are careful to point out many limitations of their paper. They also appropriately avoid describing the potential relationship between HCQ and diabetes prevention as causal, instead describing an association. This difference is subtle but important, as pharmaco-epidemiology cannot prove causation. This paper should be viewed as hypothesis generating. Proof of this hypothesis will rely on more detailed clinical pharmacologic studies to assess HCQ’s effect on blood sugar. Also, randomized controlled trials of HCQ among patients with borderline blood sugars (with or without RA) should be considered. Until I see these types of data about HCQ, I will not change my prescribing practice. If this association is causal, we will be able to add an important benefit to HCQ’s resume.
References
- Petri M, Lakatta C, Magder L, Goldman D. Effect of prednisone and hydroxychloroquine on coronary artery disease risk factors in systemic lupus erythematosus: a longitudinal data analysis. Am J Med.1994;96:254-259.
- Shojania K, Koehler BE, Elliott T. Hypoglycemia induced by hydroxychloroquine in a type II diabetic treated for polyarthritis. J Rheumatol. 1999;26:195-196.
- Quatraro A, Consoli G, Magno M, et al. Hydroxychloroquine in decompensated, treatment-refractory noninsulin-dependent diabetes mellitus. A new job for an old drug? Ann Intern Med. 1990;112:678-681.
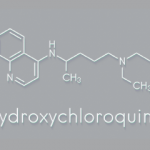
HCQ Has Many Benefits for Lupus Patients
By Joan M. Von Feldt, MD Alarcon GS, McGwin G, et al. Effects of hydroxychlorquine on the survival of patients with SLE: data from LUMINA a multi-ethnic US cohort (LUMINA L). Ann Rheum Dis. 2007;66:1168-1172.
Abstract
Objective: In patients with systemic lupus erythematosus (SLE), HCQ prevents disease flares and damage accrual and facilitates the response to mycophenolate mofetil in those with renal involvement. A study was undertaken to determine whether HCQ also exerts a protective effect on survival.