TNF Agonists and Mortality
By Daniel Hal Solomon, MD, MPH
Carmona L, Descalzo MA, Pérez-Pampín E, et al. All cause and cause-specific mortality in rheumatoid arthritis are not greater than expected when treated with TNF antagonists. Ann Rheum Dis. Online before print. February 26, 2007. doi:10.1136/ard.2006.067660.
Abstract
Background: Mortality is increased in RA mainly due to cardiovascular events, cancer, and infections. Recent data suggest that treatment with tumor necrosis factor (TNF) antagonists may affect this trend.
Objective: To assess whether treatment with TNF antagonists is associated with reduction in cardiovascular events, cancer and infection rates, and in mortality in RA patients treated compared with those not treated with TNF antagonists.
Methods: BIOBADASER is a registry for active long-term follow-up of safety of biological therapies in rheumatic patients. It includes 4,459 RA patients treated with TNF antagonists. EMECAR is an external RA cohort (n=789) established to define the characteristics of the disease in Spain and to assess comorbidity. The incidence density (IHD) of cardiovascular events, cancer, and infections was estimated and compared in both cohorts. The Standardized Mortality Ratio (SMR) was compared with the rate in the general population. A propensity score was used to match cohorts by the probability of being treated.
Results: Rates of cardiovascular and cancer events are significantly higher in EMECAR than in BIOBADASER (Rate ratio [RR]=5 to 7 for different cardiovascular events, and RR=2.9 for cancer), whereas rate of serious infections is significantly higher in BIOBADASER (RR=1.6). Mortality-rate ratio of BIOBADASER by EMECAR is 0.32 (0.20–0.53) for all causes of death, 0.58 (0.24–1.41) for cardiovascular, 0.52 (0.21–1.29) for infection, and 0.36 (0.10–1.30) for cancer-related deaths.
Conclusion: Morbidity (other than infection) and mortality are not higher than expected in patients with RA treated with TNF antagonist.
Commentary
BIOBADASER and EMECAR researchers investigate a topic of great concern: whether TNF antagonists are associated with excess mortality in patients with RA. Because trials of TNF antagonists are relatively small and short in duration, this question will best be answered by careful epidemiologic studies. To this end, the current analyses compare all-cause and cause-specific mortality among patients with RA treated with and without a TNF antagonist. While we should probably accept the conclusion that there is no greater mortality risk among TNF-antagonist users, the assertion that all-cause mortality may actually be reduced in this group warrants careful inspection.
These investigators have systematically collected data on outcomes in two national registries of RA. BIOBADASER has enrolled TNF-antagonist users and EMECAR synthetic–disease-modifying antirheumatic drug (DMARD) users. Information collected in these two registries is similar but not identical, and many of the same clinical centers participate in both registries. The difficult methodological issue for this analysis is ensuring the comparability of the study groups. While this goal sounds simple, it turns out to be quite difficult even for established epidemiologists. It may even be more difficult in countries where regulators restrict use of expensive TNF antagonists to certain types of patients, almost ensuring that the two groups will not be comparable. These restrictions usually focus on RA disease activity measures. However, even more problematic than non-overlap in RA disease activity is the possibility of different distributions of comorbid conditions. Patients with severe RA who are not prescribed a TNF antagonist often have comorbidities that make clinicians and patients cautious about using an infusion or injectable medication with an incompletely understood side-effect profile.
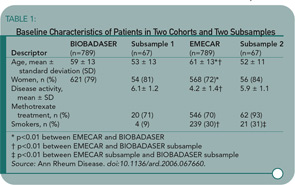
These methodologic issues were apparent to the investigators, but is it unclear how completely this potential source of bias was managed in their analyses. Recognizing potential differences in the two cohorts, the investigators created two propensity-matched cohorts. They matched patients on their probability of receiving a TNF antagonist. These sub-samples are better matched than the parent cohorts on age, gender, and Disease Activity Score, but they are not well matched with respect to methotrexate use and smoking habit (see Table 1, above right). Moreover, the percentage of patients and sample sizes suggest that many patients have missing data (see methotrexate for an example). The propensity score method can be quite useful when it produces comparison groups well balanced on relevant confounders; however, Table 1 demonstrates that the matched subsamples are not adequately balanced.
The authors then compare the samples from the parent cohort to calculate rate ratios. They note a significantly reduced all-cause mortality-rate ratio for the TNF antagonists compared with synthetic-DMARD users. However, based on the imbalances in the parent cohort, these comparisons are of limited value. The unadjusted rate ratios from the propensity-matched cohorts are also of limited value because of the recognized differences in smoking habits. Moreover, the lack of information on many other potentially important covariates makes it impossible to evaluate the validity of any of their comparisons.
This paper is valuable in stating that there is no increase in mortality associated with TNF antagonists. However, statements about a reduction in mortality are not clearly supported by their data. Valid comparisons can only be made between groups that overlap in their characteristics, thus allowing for adjustment in regression analyses. While registries will enhance our understanding of the safety and effectiveness of RA treatments, we have not yet established valid methods for studying registries.
Catalogue the Complexity of RA Care
By Michael M. Ward, MD
Kahn KL, MacLean CH, Liu H, et al. The complexity of care for patients with rheumatoid arthritis: metrics for better understanding chronic disease care. Med Care. 2007;45(1):55-65.
Abstract
Background: Patients with RA provide an important opportunity for understanding care of patients with a serious chronic condition.
Objective: We sought to characterize the complexity of care for patients with RA, including metrics describing the patient, the disease, and use of the healthcare system across time and place.
Methods: We undertook a prospective cohort study of 568 community-dwelling patients with RA by using observational data from clinically detailed telephone interviews at baseline and two years later in addition to medical record abstraction. Health status, comorbidity, use of DMARDs, visits, providers, provider types, encounter settings, and the discontinuity between patients and providers were studied.
Results: Within a 12-month window, 568 patients had 8,686 outpatient encounters with the healthcare system with a mean of 3.41 unique providers per patient associated with a mean of five primary care and six rheumatologist visits. Half did not see a primary care physician and 20% did not see a rheumatologist during six-month periods, despite their use of potentially toxic drugs, a mean of four comorbidities, and progressive RA. Over the course of 24 months, 29% of patients changed their primary care provider, and 15% changed their rheumatologist. Patients were moderately impaired with mean SF-12 physical component score 37 (standard deviation, 9).
Conclusion: Patients with RA have frequent encounters with multiple providers and also frequent discontinuity of care. Recognizing the complexity of the care of patients with a chronic disease across multiple dimensions provides an opportunity to better understand challenges and opportunities in delivering high-quality care.
Commentary
Making decisions on follow-up appointments, asking for consultations, returning patient telephone calls, communicating with primary care physicians, and transferring medical records to other providers are part of the mechanics of clinical practice. Although most of us live it on a daily basis, rarely do we step back and consider how these efforts fit into the overall pattern of patient care. This study attempts to do just that in a survey of healthcare use by 568 patients with RA.
In a prodigious effort of patient interviews and medical record reviews conducted in 2001, the investigators cataloged the type and frequency of contacts these patients had with healthcare providers during one year.
Some findings were not surprising. Patients with RA are frequent users of healthcare, although the annual number of visits among patients in this study (mean of 4.5 visits to a primary care provider and 5.5 visits to a rheumatologist) was slightly lower than those of past studies. Eighty-six percent of patients saw a rheumatologist during the year before the survey, and 69% did so during the three months before the survey. This frequency was not likely skewed by the study’s source population or recruitment strategy, as most subjects were identified from insurance claims or laboratory databases, and only 15% were recruited from rheumatology practices.
Other findings are more interesting. More than 20% of patients had at least one appointment cancellation or no-show (to any provider, not necessarily to rheumatologists). Only about 20% had at least one visit with a physician assistant or nurse practitioner. These observations suggest opportunities to improve the efficiency of care. In contrast, 37% of patients had a visit that was classified as unscheduled, urgent, or emergent.
Most interesting was the information obtained on a follow-up survey conducted two years later. During this time, 29% of patients changed their primary care provider and 15% of patients changed their main arthritis doctor (who was not necessarily a rheumatologist). The most common reasons for this were the patient or provider moved (29%), the patient was not happy with the provider (13%), or because of insurance restrictions (10%). What consequences these changes might have had on coordination of care, treatment plans, or health outcomes was not studied.
Given that the patients studied had medical insurance, these results may be somewhat biased toward a more favorable assessment than exists in the population as a whole. Patients without insurance or those with public insurance may have less access to specialists and greater fragmentation of care than the patients who were studied. This study does not describe the nature of the care provided during visits or link the process of care to patient outcomes. The study also does not attempt to describe what types of care are appropriate or inappropriate, or useful or wasteful, but highlights the diversity of sources of care that characterize current clinical practice.