Both arthralgias and frank arthritis can occur. Initially, these tend to be transient and mild in an oligoarticular distribution: knees, wrists, ankles, elbows, shoulders and PIP joints. However, these conditions may evolve over months to a severe and destructive polyarthritis resembling rheumatoid arthritis. Radiographic evidence of wrist fusion is very characteristic, but rare (see Figure 2).

Figure 2.
Wrist Fusion
In addition to the classical triad of fever, rash and joint pain, a variety of gastrointestinal manifestations can occur. Abdominal pain occurs in up to half of patients, and nausea, anorexia and weight loss can occur. More serious problems include aseptic peritonitis, acute pancreatitis and lymphadenitis. Hepatomegaly can occur, and modest elevations of transaminases are common. Eight cases of fulminant liver failure have occurred, with four fatalities. Splenomegaly occurs in up to half of patients, as does cervical lymphadenopathy.
Cough, dyspnea and pleurisy can occur. Pleural effusions, pericarditis, myocarditis, arrhythmias, tamponade and interstitial pulmonary infiltrates may occur. The adult respiratory distress syndrome can occur in the setting of the macrophage activation syndrome. Aseptic meningitis, sensorineural hearing loss and microangiopathic hemolytic anemia can occur.
The macrophage activation syndrome (i.e., hemophagocytic syndrome) was reported in 12% of 50 patients.1 This presents with leukopenia, thrombocytopenia, very high serum triglycerides, and normal or low haptoglobin and fibrinogen. A bone marrow exam shows hematopoietic cells undergoing phagocytosis by macrophages.
Disease course can be quite variable, not only in severity, but in terms of pattern. A monophasic pattern, with fever, rash, serositis and hepatosplenomegaly, runs a course of weeks to months, usually resolving within a year. An intermittent pattern entails remissions and exacerbations over months to years. Subsequent flares tend to be shorter and less severe. Finally, the chronic pattern involves persistently active disease with articular symptoms and, sometimes, destructive arthritis.
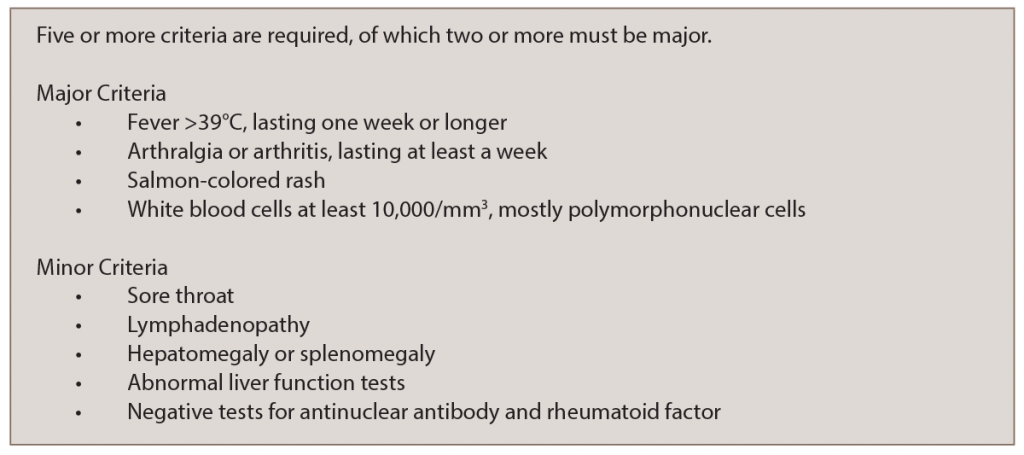
AOSD is a clinical diagnosis, which requires exclusion of infectious and malignant causes of fever. The Yamaguchi Criteria (see Table 1) are met by the presence of five criteria, of which two must be major.2 However, such criteria are not absolute, and in the end, it is the clinical judgment of the physician that establishes the diagnosis.
The pathophysiology of ADS is obscure. It has been hypothesized to be a reactive process to an infection (like many other rheumatologic diseases). Inflammatory cytokines, such as interleukin 2 (IL-2), interferon gamma (IFN and tumor necrosis factor-alpha (TNFα), are present in substantial amounts: biologic DMARDs targeting TNFα and other cytokines are sometimes effective treatments.
Autoimmune vs. Autoinflammatory Diseases
Rheumatologists are familiar with autoimmune diseases, such as lupus, Sjögren’s syndrome, etc., which are mediated by T and B cells of the adaptive immune system. A vaccination produces a reaction from the adaptive immune system to produce protective antibodies. Autoantibodies are associated with autoimmune diseases in many cases.