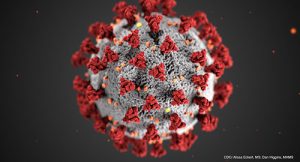
 Humans may fear change as a general rule, but we’re adaptable when we need to be. In this era of COVID-19 and social distancing, medical practices and payers are adapting to an increased use of telemedicine, which enables providers to see their patients without being in a room with them.
Humans may fear change as a general rule, but we’re adaptable when we need to be. In this era of COVID-19 and social distancing, medical practices and payers are adapting to an increased use of telemedicine, which enables providers to see their patients without being in a room with them.
To cope, the Centers for Medicare & Medicaid Services (CMS) and commercial payers have relaxed their rules regarding telemedicine.1,2 Things are still evolving, so it’s important for rheumatology practices to stay up to date on the appropriate billing codes—including new codes from the International Classification of Diseases, 10th Edition (ICD-10) related to COVID-19—and other guidelines surrounding telemedicine. ACR staff is monitoring these changes and has compiled a collection of online resources to help practices glean the most important details.
Telemedicine Expansion
Before the current public health emergency, rheumatologists could practice telemedicine only in certain circumstances, such as to help patients in rural areas. But with stay-at-home orders being issued across the country, it became necessary for the CMS and other payers to update their guidelines so physicians could safely continue treating patients.
On March 17, the CMS announced expanded allowances for telemedicine on a “temporary and emergency” basis. Most third-party payers—including the big four, UnitedHealthcare, Aetna, Cigna and Blue Cross Blue Shield—have followed suit.3-6
The CMS specifies three main categories of telemedicine appointments that can be submitted for reimbursement:
- Telehealth is a visit with a patient in which the provider uses an audio-video or audio-only telecommunications system;
- A virtual check-in is a brief check-in with a patient using a recorded video and/or images submitted by the patient; and
- An electronic visit, or e-visit, is communication with a patient through an online patient portal.
The ACR Telehealth Provider Fact Sheet and FAQ provide an overview of telemedicine, including information on billing and coding, licensure, state actions and more.7
Telemedicine Coding & Billing
With the expanded use of telemedicine, medical practices need to adjust their coding and billing procedures. This includes using the new ICD-10 codes related to COVID-19, as well as following new and evolving rules regarding place of service codes and modifiers for telemedicine.
Keep in mind that the CMS and the various commercial payers handle their updated rules differently, says Antanya Chung, CPC, CPC-I CRHC, CCP, ACR director of practice management. She and other staff at the ACR investigated these variations in compiling the ACR Telehealth Coding Reference, a quick reference guide intended to help rheumatology practices navigate telehealth coding and billing requirements.8


