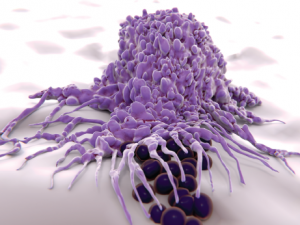
Macrophages engulf and digest cellular debris and pathogens.
Juan Gaertner / shutterstock.com
MADRID—Research into pharmacodynamic biomarkers has shown that macrophages may have an important role in the pathogenesis of several diseases, including systemic sclerosis, an expert said at the 2017 Annual European Congress on Rheumatology (EULAR). The findings were discussed in a session that also covered how an understanding of M1 macrophages’ role in fibrosis has evolved from kidney research.
Robert Lafyatis, MD, director of the University of Pittsburgh Scleroderma Center, said that when his lab has looked at genes implicated in a variety of diseases, genes related to macrophages have figured prominently over and over again.
Researchers took skin biopsies from the forearm and looked at genes that correlated with the modified Rodnan skin score (mRSS) for the whole body. In addition to the types of genes they expected to find, researchers saw that macrophage-related genes were clustered together, highly correlated with the mRSS. “That’s what made us think that macrophages may be important to skin diseases, [such as] systemic sclerosis,” Dr. Lafyatis said.
When researchers tracked data over time, they found that as the skin score worsened, expression of these genes—including thrombospondin-1 and MS4A4A—was increased. It was a longitudinal biomarker they found so reliable that it’s now used in clinical trials.
They’ve also looked at tocilizumab trial data from patients receiving placebo and found that macrophage-related genes were linked to changes in a patient’s skin score. “Macrophage markers appear prominently in our pharmacodynamics biomarkers [and] in our prognostic biomarkers,” Dr. Lafyatis said. “In other words, the number or some quality of macrophages seems to be an important predictor, if you will, of whether somebody’s going to develop progressive skin disease.”
The expression of these genes is also correlated with systemic sclerosis-related interstitial lung disease, researchers found.
‘Metabolism is relevant in understanding how macrophages work,’ Dr. Camara said.
“From several different standpoints—skin disease, interstitial lung disease, pulmonary hypertension—we see this recurrent theme of macrophages somehow having an important role in pathogenesis—or at least the most obvious role,” he said. However, what activates them remains unclear.
“There are lots of different kinds of macrophages and dendritic cells in different sites,” Dr. Lafyatis said. “They’re different at different sites. They’re different when they start, and then they’re going to change. That’s one of the questions: How do they change as you have disease come on? All of these things are difficult questions to answer.”
