Similarly, ACPA of the IgA isotype have been found in the sputum of seronegative individuals at risk for developing RA, supporting a mucosal origin of ACPA, which may be influenced by resident microbiota.9 In the intestine, Prevotella copri is expanded in the feces of newly diagnosed, untreated patients with RA, compared with those with established disease and healthy controls.10
In spite of the strong correlative data between disease and microbiome changes, identifying a causative role for the microbiome to stimulate immune changes that lead to RA remains elusive. The mechanism in which microbial changes influence disease is still unclear, and hypotheses include molecular mimicry, creation of an inflammatory environment that changes immune function, moderating nutrient absorption or modifying proteins secreted by human cells.
Future studies will need to aim at identifying bacterial interactions with host mucosa and downstream immune alterations leading to disease development to provide a causal link between dysbiosis and RA.
Spondyloarthritis (SpA)
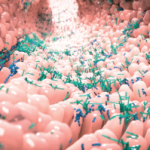
The idea that changes in gut homeostasis influence the development of seronegative arthritis, termed gut–joint hypothesis, also has notable indirect evidence. About 32% of individuals with inflammatory bowel disease (IBD), a condition with well-established intestinal dysbiosis, have radiographic evidence of axial arthritis, and 18–45% will develop symptoms related to joint inflammation.11,12 Reactive arthritis (ReA), which can be caused by gastrointestinal infections with gram-negative bacteria, provides more clinical evidence of the gut–joint hypothesis. Fragments of the ReA-associated organisms that originate in the colon, Yersinia and Salmonella, have been found in the synovium of patients with ReA.13 Cell culture studies have demonstrated that HLA-B27 cells are more readily infected with Salmonella, and gut-derived monocytes and T cells can be found within the joints of those with SpA.14-17 Consequently, microbe–host interactions in the intestine appear connected to joint pathophysiology.
Microbiome studies of individuals with psoriasis find reduced cutaneous bacterial diversity and partial normalization after treatment with systemic therapies.18 However, preliminary data presented as an abstract at the 2015 ACR/ARHP Annual Meeting suggest that there are no differences between the skin microbiome of individuals with psoriasis and those with psoriatic arthritis, suggesting that the dysbiotic populations driving arthritis are unlikely to be cutaneous.19
In the intestine, patients with either psoriasis or psoriatic arthritis both have decreased fecal Coprococcus compared with healthy controls, but individuals with psoriatic arthritis also have increases in certain bacterial taxa that were not observed with psoriasis alone.20 Unfortunately, the specific effect of Coprococcus on host physiology is unknown, but it’s likely mediated through the production of short-chain fatty acids, some of which are known immune regulators.21,22