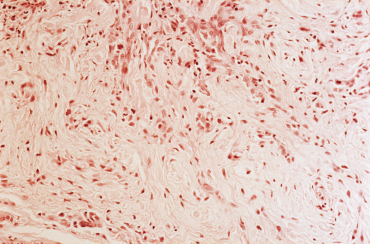
Lichen myxedematosus and scleromyxedema.
Biophoto Associates / Science Source
Scleromyxedema is a rare, mucinous skin disorder of unknown origin, one of a number of conditions that mimic systemic sclerosis. Although cases of scleromyxedema remain rare, a better understanding of its mechanisms of action could have implications for the research and treatment of scleroderma and related autoimmune conditions, says Laura K. Hummers, MD, ScM, co-director of the Scleroderma Center at Johns Hopkins University School of Medicine, Baltimore.
“We don’t know the actual prevalence of scleromyxedema, in part because rheumatologists don’t always think to look for it,” says Dr. Hummers, corresponding author of an open-label, observational report on 15 patients with scleromyxedema and the impact of intravenous immunoglobulin (IVIG) therapy published in the journal Arthritis Care & Research.1 “When I reviewed the indexed medical literature, I found a total of 200 cases referenced, mostly case reports.”
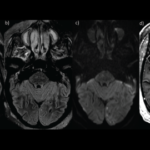
This potentially life-threatening systemic disorder is associated with profound central nervous system disturbances, including seizures and coma, and can also involve inflammatory polyarthritis, proximal myopathy and gastrointestinal abnormalities. Scleromyxedema has a similar distribution of skin findings as systemic sclerosis, with similar clinical features such as arthritis, Raynaud’s syndrome, skin fibrosis and esophageal dysmotility in some patients.
Scleromyxedema has no approved diagnostic criteria or diagnostic codes. “We don’t know the cause, although it is universally associated with monoclonal proteins. But how that connects with other aspects of the disease is not clear,” Dr. Hummers says. All but one of the 15 patients she studied had monoclonal gammopathy of undetermined significance in their blood plasma.
Franco Rongioletti, MD, chair of the Unit of Dermatology at the University of Cagliari, Italy, and colleagues have also reported on case studies of European scleromyxedema patients and progress in developing diagnostic criteria and lines of treatment.2 They found monoclonal gammopathy in 27 of 30 patients and confirmed that scleromyxedema is a chronic and unpredictable disease with severe systemic manifestations and a guarded prognosis.
Treatment Almost Always Succeeds
“What landed scleromyxedema on my plate at the Scleroderma Center is that we had seen a couple of case reports about its treatment with intravenous immunoglobulin (IVIG). Then we picked up a few patients of our own and successfully treated them with IVIG,” Dr. Hummers tells The Rheumatologist.
But immunoglobulin comes with complications, including potential for blood clotting during treatment. A bigger problem? Its high cost, up to $15,000 per treatment, initially given monthly. “We also need to infuse it very slowly. It takes two to five days, with a home healthcare nurse present, to administer a single dose,” says Dr. Hummers.

Dr. Hummers
Although much about this condition remains a mystery, IVIG almost always succeeds as a treatment for scleromyxedema, at least initially according to Dr. Hummers. Some patients may require adjunctive therapies, “but we don’t know why. If we knew what changed in the body as a result of IVIG therapy—immune system, gene expression, skin disturbances—that could help guide future research,” she says. “We wanted to see whether IVIG therapy would introduce measurable biologic effects.”
The Hopkins study recruited 15 Scleroderma Center patients prescribed IVIG. Clinical data and biopsies were gathered immediately before IVIG treatment, and again one to two weeks after. Peripheral blood mononuclear cells were obtained for flow cytometry. The clinical information included a modification of the modified Rodnan Skin Score (mRSS) to assess skin thickness, patient-reported skin outcomes and the Health Assessment Questionnaire-Disability Index. Noted treatment effects included reduction in mRSS from 13.6 ±2.6 to 10.3 ±1.9, along with improvements in skin flexibility and softening and in patient-identified visual analog scales for skin pain and itching.
“It’s pretty clear IVIG achieves positive outcomes, both objectively and subjectively,” Dr. Hummers says. Molecular analysis of RNA in skin tissue following treatment showed decreased gene expression of transforming growth factor beta (TGFβ) cytokines and interferon-inducible proteins.
What Should Rheumatologists Look For?
Diagnostically, scleromyxedema is not a big challenge to identify if the doctor knows to look for it, Dr. Hummers says. “It’s important for rheumatologists evaluating patients for scleroderma to consider it. It has a particular predilection for skin abnormalities on the face, around the ears and at the middle of the back.”
The skin disturbances caused by scleromyxedema also tend to have a bumpy quality, in contrast to scleroderma, in which the affected skin is thickened but usually flat. And it involves deposits of mucin, unlike scleroderma, which involves collagen deposits. “But if you don’t ask for a special stain for mucin in the biopsy, it likely won’t be tested for,” says Dr. Hummers.
Scleromyxedema is rare enough that it probably won’t be the target of a clinical trial. “But we were in a unique situation where we have a treatment for this rare disease, we know it works in almost all cases, but we don’t know how it works. We thought we should take advantage of that unique situation to study this rare condition. This was a small study with a big gene expression analysis,” she says.
“Maybe we’ll learn something about scleroderma and the other mimics. We got a few signals from our research about future directions to pursue,” she adds. The biologic studies also suggest there may be a role for T lymphocytes in the pathogenesis of the disease.
Dr. Rongioletti told The Rheumatologist in a recent email that scleromyxedema requires a multi-disciplinary approach to treatment. “Dermatologists are often the first specialists to see these patients and to make the diagnosis of this disabling and potentially fatal condition, whose therapy is challenging,” he said. From his European multi-center study of 30 patients with scleromyxedema and from a personal trial on eight patients, Dr. Rongioletti concludes IVIG can be successful, even though maintenance infusions are required to control the disease.3
“The new study from the group led by Dr. Hummers, who is an expert in this field, has confirmed that patients with scleromyxedema benefit from IVIG,” he noted. The study also sheds light on the pathogenesis of this mysterious disease, characterized by immunological disturbances. The role for T lymphocytes and for some cytokines, such as TGFβ, and interferon pathways should be considered for future therapeutic approaches.
Larry Beresford is a medical journalist in Oakland, Calif.
References
- Mecoli CA, Talbot CC Jr, Fava A, et al. Clinical and molecular phenotyping in scleromyxedema pre- and post-treatment with intravenous immunoglobulin. Arthritis Care Res (Hoboken). 2019 Apr 22. [Epub ahead of print]
- Rongioletti F, Merlo G, Cinotti E, et al. Scleromyxedema: A multicenter study of characteristics, comorbidities, course, and therapy in 30 patients. J Am Acad Dermatol. 2013 Jul;69(1):66–72.
- Guarneri A, Cioni M, Rongioletti F, et al. High-dose intravenous immunoglobulin therapy for scleromyxedema: A prospective open-label clinical trial using an objective score of clinical evaluation system. J Eur Acad Dermatol Venereol. 2017 Jul;31(7):1157–1160.