Phantom Pain and Ocular Pain in SS
As noted earlier, ocular symptoms in patients with SS are out of proportion with objective observations of the ocular surface, largely due to the mysterious perception of “phantom pain.”
The concept of “phantom pain” may arise at the level of the cranial nerve, spinal dorsal root ganglia, and thalamus or brain cortex. As noted above, these processes may be strongly influenced by local release of cytokines by microglial cells.3 This observation correlates with our clinical observation that the pain and discomfort in patients with SS whose disease is longstanding is much less improved following treatment with biologic agents than in patients with early disease.
Phantom pain explains the aberrant, painful ocular sensation that chronic post-Lasik patients or patients with SS experience when they report that their pain is only partially relieved by a topical anesthetic.
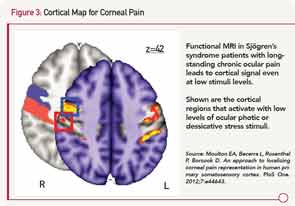
Sites for ocular pain have been mapped by functional magnetic resonance imaging to a specific region of the prefrontal cortex (see Figure 3).15
To emphasize, a patient’s complaints of pain derive not only from the pain fiber on the surface of the eye, but also from the part of the brain where that sensation is processed and remembered. Thus, a new frontier for therapy will be the understanding of noxious stimuli from primary somatosensory cortex that involves alpha-delta fibers.16
I began following the simple procedure of Rosenthal et al in our rheumatology clinic by asking patients with SS about their ocular pain level at their routine exams. Not unexpectedly, patients with longstanding disease would report their pain level to be a seven or 8 on a scale of 10. What was surprising was that patients reported their pain level had diminished only slightly, to a 4 or 5 score after instillation of a topical anesthetic into the eye. There is little doubt that the anesthetic was effective, since the corneal reflex (the blink after gentle pressure to cornea) was obliterated indicating loss of the afferent loop of the reflex.
In summary, it appears that a patient with an acute insult to their eye (such as a corneal abrasion) may have significant, although temporary improvement in ocular discomfort with a topical anesthetic. However, the patient with SS who has chronic eye pain does not obtain the same relief from anesthetic. The simplest explanation is that patients with SS develop a phantom pain as the result of the chronic ocular irritation.