Kateryna Kon / shutterstock.com
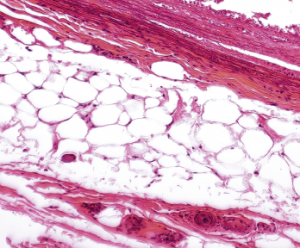
AMSTERDAM—It’s been many years since adipose tissue came to be appreciated not just as a store of energy, but also as a regulator of metabolism and an important player in immune function. Rheumatology researchers continue to drill down into the role of fat cells in the search for mechanisms that could reveal targets for the treatment of rheumatic diseases, and experts shared recent findings in a session at EULAR: the Annual European Congress of Rheumatology.
Response to the Western Diet
Henk Schipper, MD, PhD, a pediatric cardiology fellow at University Medical Center Utrecht in The Netherlands who specializes in the study of adipose tissue, said the understanding of adipose tissue has continued to deepen over the past 30 years, with such milestones as the discovery of the hormone leptin and adipose tissue macrophages. The volume of work in the field has soared.
Recently, an international group of investigators found that mice on a high-fat, high-glucose Western diet showed a more aggressive response to stimulation with lipopolysaccharide (LPS) than control mice, but that this response was long lasting—seen again weeks after the mice were put back on a normal chow diet.1 This lasting response must mean the Western diet causes a fundamental change in the mice, the researchers say.

Dr. Schipper
“What they claim in this paper … is that there must be transcriptomic, epigenomic changes induced by the Western diet to really have long-lasting effects on the response of the immune cells,” Dr. Schipper said. “This is definitely something that’s also relevant for many rheumatoid disorders.”
Dr. Schipper said he is optimistic about the potential for therapeutic breakthroughs that can repair the “holes” that arise when the relationship between fat tissue and immune function is disrupted.
“There has been a huge increase in papers dealing with adipose-tissue immunology, adipose-tissue inflammation and immune-metabolism over the last few decades,” he said. “This is supposed to be the era of translation. Hopefully in the next few years we’ll see a lot of trials—and successful trials—to fix these holes in the co-evolution of adipose tissue and immunology.”
‘There must be transcriptomic, epigenomic changes induced by the Western diet to really have long-lasting effects on the response of the immune cells,’ Dr. Schipper said.
Adipokines
Silvia Bosello, MD, PhD, professor of rheumatology at the Catholic University of the Sacred Heart in Rome, presented findings on how adipokines—proteins produced by white adipose tissue that are involved with endothelial cell homeostasis and angiogenesis and that regulate the immune response and systemic inflammatory process—are reduced in systemic sclerosis (SSc).2
Researchers assessed three types of adipokines—chemerin, leptin and adiponectin—in 100 SSc patients and 30 matched controls. They found all three types of adipokines were reduced in the SSc patients.
They also found that adipokine levels directly correlated with a more aggressive pattern on nailfold videocapillaroscopy.
Further, they found, patients with greater lung capacity—a diffusion level of carbon monoxide of at least 50%—had higher levels of adiponectin than patients with lung capacity below that threshold.
The downregulation of adipokines in the context of more severe disease, Dr. Bosello said, “suggests a possible role of chemerin, leptin and adiponectin in the impaired angiogenesis and in the development of vasculopathy of SSc patients.”
Fat-Associated Lymphoid Clusters

Dr. Caamaño
Jorge Caamaño, PhD, a reader in cellular immunology at the University of Birmingham in the U.K., discussed his group’s latest findings on fat-associated lymphoid clusters (FALCs)—platforms that form quickly after infection or injury to help coordinate interaction among immune cells, and that support innate and adaptive immune responses.3
The group has recently shown that bacteria and helminth infections bring about a big increase in the number of FALCs, with recruitment of B and T lymphocytes and macrophages.
Dr. Caamaño suggested that immune lymphoid cells, a group of innate immune cells, in FALCs are early responders to intestinal infections and spur expression of cytokines, depending on the infecting agent and the metabolism of the host. Their work is continuing.
“It is essential to understand the mechanisms that induce FALC formation and their function in intestinal infection and inflammation,” Dr. Caamaño said, “in order to facilitate immune responses and to control the deleterious reactions during chronic inflammatory diseases.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Christ A, Gunther P, Lauterbach MAR, et al. Western diet triggers NLRP3-dependent innate immune reprogramming. Cell. 2018 Jan 11;172(1–2):162–175.e14.
- Bosello S, De Lorenzis E, Canestrari G, et al. Adipocytokines imbalance is associated with vascular damage in systemic sclerosis [abstract OP0107]. Ann Rheum Dis. 2018 Jun 14;77(suppl):A104.
- Cruz-Migoni S, Caamaño J. Fat-associated lymphoid clusters in inflammation and immunity. Front Immunol. 2016 Dec 21;7:612.
