AB Visual Arts / shutterstock.com
Preventing adverse outcomes in individuals who have rheumatic diseases is a daily goal for rheumatologists. For example, rheumatologists prescribe medications and perform screening to prevent erosions in rheumatoid arthritis (RA), renal failure in systemic lupus erythematosus and flares across all diseases. Many of these actions are classified as secondary or tertiary prevention, because individuals have already presented with clinical signs and symptoms of disease (e.g., swollen and tender joints, nephritis), and often meet established classification or diagnostic criteria. In addition, rheumatologists often try to prevent other adverse outcomes through approaches classified as primary or secondary prevention. These approaches include vaccinations for immunocompromised individuals, use of bisphosphonates in individuals who are at high risk of fracture on the basis of low bone mineral density, and statin use in individuals with rheumatic diseases with high risk for cardiovascular disease based on objective biomarkers, such as elevated cholesterol.
However, it is less common for rheumatologists to treat with medications to prevent the onset of a primary rheumatic disease based solely on a biomarker or other risk factor—for example, preventing the onset of inflammatory arthritis in someone with rheumatoid factor (RF) and/or anti-citrullinated protein/peptide antibody (ACPA) positivity, psoriasis or the first episode of gout in an individual with very elevated serum uric acid. Traditionally, many rheumatologists are deeply rooted in the concept, “Don’t treat a test; treat the patient,” and await clinically apparent signs of disease prior to initiating treatment.
Studying Disease Prevention
For some primary rheumatic diseases, the approach to preventing the first flare of disease may be changing. Several trials now underway or recently completed seek to prevent or delay the first appearance of clinically apparent synovitis in RA.
One of these trials, PRAIRI (Prevention of Clinically Manifest Rheumatoid Arthritis by B Cell-Directed Therapy in the Earliest Phase of the Disease), was based in the Netherlands and was completed in 2016. Although a peer-reviewed manuscript has not yet been published, the study’s results were reported at scientific meetings.1 This study identified individuals who were positive for anti-citrullinated protein/peptide antibody (ACPA) and rheumatoid factor (RF) without evidence of synovitis at baseline and randomly assigned them to receive a single dose of rituximab (1,000 mg) or placebo. Approximately 80 subjects were randomized, but overall rates of development of RA (~40%) were similar between treated and untreated patients. However, the onset of inflammatory arthritis was delayed by ~12 months in the treated subjects.
Several other RA prevention trials underway have similar inclusion criteria. In the U.S., the three-year StopRA (Strategy for the Prevention of Onset of Clinically Apparent RA) study is randomizing individuals with ACPA positivity of two times or greater the upper limit of normal, but with no history of synovitis, to receive hydroxychloroquine or placebo for 12 months followed by 24 months of drug-free observation. The primary endpoint is the development of classifiable RA under the 2010 ACR/European League Against Rheumatism (ACR/EULAR) Classification Criteria.2,3 In the United Kingdom, the APIPPRA (Arthritis Prevention in the Pre-Clinical Phase of RA with Abatacept) trial includes individuals with positivity for both ACPA and RF, or ACPA at three times or more of normal, as well as joint symptoms that appear inflammatory, but without joint examination findings of synovitis at baseline.4 The intervention in APIPPRA is abatacept (or placebo) for one year, with an additional year of follow-up.
Several other trials are underway or in development to evaluate a variety of other agents, including statins and methotrexate, in similar autoantibody positivity populations without inflammatory arthritis or populations with signs and symptoms of early inflammatory arthritis but no classifiable RA.5,6
The rationale for performing these trials is based on several factors. The first is that ACPA positivity, especially at high levels, is highly predictive of developing RA. This is based on several retrospective case-control studies where ACPA positivity with or without RF positivity have demonstrated high rates (typically >90%) of progression to RA compared with antibody negative individuals.7-9 In addition, several prospective studies have shown that ~40–60% of ACPA-positive individuals develop inflammatory arthritis and/or classifiable RA over ~two to five years of follow-up—time frames that are feasible to study in clinical trials. Even higher rates of RA progression may be seen in certain individuals, such as those with even higher levels of ACPA, concomitant positivity for RF and greater degrees of joint symptoms. Other factors, such as ongoing smoking and obesity, and genetic factors, such as the shared epitope, also contribute to the progression of RA among patients with ACPA positivity.10-13
A growing number of other studies also demonstrate that early treatment of clinically apparent RA leads to improved outcomes and, perhaps, long-term drug-free remission.14 Because patients have evidence of altered immunity well before clinical presentation, this may imply that initiating therapy prior to the first clinical flare may have potential for long-term benefits, such as delay in first flare, a milder disease course or even prevention of disease altogether. Importantly, while the specific drug or duration of therapy ‘ideal’ to use in RA prevention is not clear, all the agents that have been or are being studied for RA prevention have been approved for use in clinically apparent RA and are generally well tolerated. Thus, they hold promise to be safe and effective in RA prevention. However, clinical trials will need to be completed to determine their real-life balance of efficacy, safety and tolerability when used in RA prevention.
New pharmacologic agents could be developed to target specific pathways that may be more relevant in preclinical RA, because we cannot assume that drugs that work well in the clinically apparent phase of disease are necessarily ideal for prevention.
What’s Next?
The field is awaiting the full results from these RA prevention trials. If successful, the paradigm of how RA is approached may be altered by adding prevention of the first clinically apparent flare of disease to a rheumatologist’s to-do lists. Of course, if prevention is shown in these studies to work in RA, a number of the issues discussed below will become critical to address, such as who to test and who to treat.
One of the primary issues to address is the development of methods to identify individuals who are at high risk for future RA in a large-scale, clear and cost-effective manner. This will depend to a large extent on the accuracy, availability and cost of screening approaches to identify at-risk individuals.
ACPA and RF testing, along with assessment of other factors, appears in prospective studies to identify groups in whom ~40–60% develop synovitis and classifiable RA within two to five years of follow-up. These are fairly high positive predictive values (PPVs) that are currently deemed strong enough to drive the development of clinical trials, but broad screening of the healthy population would be the next step for implementation. ACPA and RF testing are widely clinically available, so conceivably these tests could be utilized in broader screening and prevention programs.
These predictive models have been developed in relatively small populations when compared with the overall numbers of individuals worldwide with established RA, as well as the number of individuals who may be ACPA positive and not have synovitis. As such, prediction models will need to be refined as the numbers of subjects who are at risk for RA are studied as part of ongoing clinical trials and other natural history studies.
Importantly, development of screening approaches for individuals who may benefit from RA prevention also entails identifying which groups are most appropriate to evaluate. Certain populations are at increased risk for RA; therefore, these may be the groups to initially target for prevention. These groups include family members of individuals with established disease, as well as certain racial groups, such as North American natives.15,16
Predictive models for RA are being developed and refined in these clinical trials, as well as in ongoing natural history studies of the development of RA in the U.S., Canada, Europe and elsewhere.17,18 If it is shown that RA prevention works, and is cost effective and reasonably safe, general population-based approaches to identify individuals at risk for RA may be developed, such as broad ACPA testing (or testing for other biomarkers) performed routinely, much like cholesterol and hemoglobin A1c are tested (and treated) in primary care settings.
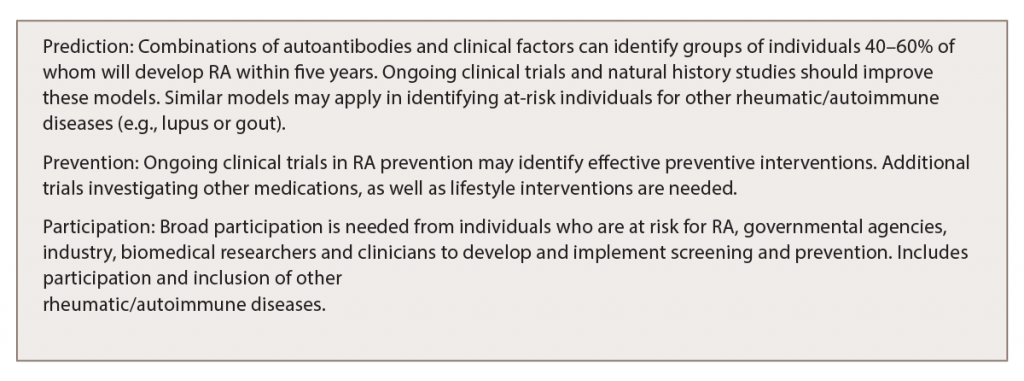
(click for larger image) Table 1: Challenges & Opportunities in Preventing RA & Other Rheumatic Diseases
Interventions
Another critical factor in prevention is to define the appropriate intervention that balances efficacy with tolerability, acceptability and cost. Several drugs are being tested in the current RA prevention trials (e.g., hydroxychloroquine, abatacept), each targeting different biologic pathways. If one of these drugs rises to the top in terms of efficacy, that may be the first agent to be used widely. However, multiple agents will likely need to be evaluated, and safety and cost would be important considerations. In addition, new pharmacologic agents could be developed to target specific pathways that may be more relevant in preclinical RA, because we cannot assume that drugs that work well in the clinically apparent phase of disease are necessarily ideal for prevention.
Alternatives to Drugs
Other factors to prevent RA are as important and effective as drugs, especially if implemented in individuals who do not yet have clinically apparent arthritis. Established and emerging evidence exists that smoking cessation may reduce RA risk, and some evidence indicates that a healthy diet, increased consumption of fish and certain other dietary factors, weight loss and exercise may reduce the risk of RA.19-22
Altered fatty acid metabolism may play a specific role in the early development RA prior to the clinical onset of synovitis.13,23 These factors will all need to be considered and studied in the context of RA prevention, although it may well be that given the potential general health benefits of many of these factors, they should be widely implemented in anyone, even those who are not at risk for RA.
Another important aspect of a preventive intervention for RA will be to determine how long the intervention needs to be applied to see benefit. For a drug, the field may hope that a short course may reset the immune system and impart lasting reduced risk. However, based on the preliminary findings from the PRAIRI study, in which disease was only delayed, as well as findings from an older study in ACPA-positive individuals in whom two doses of intramuscular corticosteroids did not halt progression to RA, it may be that drugs should be used long term to prevent clinically apparent RA.24
That approach may have challenges compared with short-term treatment in terms of adherence and potential for side effects, but it still may be beneficial for an individual if they never have a first flare of disease or other long-term adverse effects of clinically apparent RA. In addition, individuals who do not transition to clinically apparent arthritis may also be able to use a safer and potentially less expensive therapy compared with an individual who presents with more aggressive disease. For nonpharmacologic interventions, such as smoking cessation, improved lifestyle and weight loss, to have long-term benefit, these lifestyle interventions may need to be longstanding to have lasting benefit.
Motivating individuals to be assessed for their risk and to participate in preventive activities, such as medications or lifestyle changes, will be critical. This participation depends on a variety of factors, including awareness of RA as a disease and an individual’s real and perceived risk for RA, that may be influenced by predictive models and personal factors. Individual preferences for preventive treatments have been studied and found to be based on a combination of factors, including perceptions of risk and the safety and duration of an intervention.25-27
A recently completed trial randomly assigned 238 unaffected first-degree relatives to receive either an RA risk assessment, called PRE-RA, personalized to their lifestyle, RF/ACPA and genetic results, and demographic characteristics or standard information about RA without personalized results.26 At baseline, few relatives were able to identify known RA risk factors, such as smoking. However, knowledge of RA risk factors and motivation to change RA risk-related behaviors both improved during follow-up among relatives who received the personalized PRE-RA risk score compared with those who received the standard RA education. These results suggest that relatives are willing to be assessed for RA risk and that, after education, they are willing to improve their lifestyles once they understand the risk factors for RA.
Notably, factors related to the strength of a prediction estimate, and type, safety and length of therapy, apply to what an individual may be willing to do for prevention, as well as what investigators and ethical reviewers may be willing to give to an individual. For example, if a predictive model suggests an individual is at ~10% risk for the development of clinically apparent RA within the next 10 years, that individual and investigators/ethical boards may wish only to do lifestyle interventions or very safe drug therapy. Conversely, if a predictive model suggests that an individual has ~80% risk for developing clinically apparent RA within two years, an individual and investigators/ethical boards may be more willing to participate in a drug study with a therapy that may have some risk for adverse effects.
The field will also need to have clear nomenclature to define stages/phases of disease that may benefit from intervention, but perhaps do not yet meet more established classification criteria (e.g., 2010 ACR/EULAR RA Classification criteria). For example, pre-diabetes is a well understood and widely used term used to define a risk period during which interventions may reduce the risk for developing the worse disease of diabetes.28 Efforts to develop terminology that can be applied across the development of RA are not yet widely implemented and may need additional work once the natural history of preclinical RA, and the point at which lifestyle and pharmacologic interventions are best to intervene, are determined.29
The optimal metrics for judging success of an intervention, including measuring when an intervention could be tapered or possibly stopped, are also future aims for research, particularly in the prevention setting, when patients may not have symptoms. Patient-reported outcomes (including digital health), joint examinations and imaging (e.g., ultrasound) may help demonstrate that an individual has not transitioned to classifiable disease. However, blood-based biomarkers may also be highly important to follow to watch inflammation or degrees of autoimmunity—much like cholesterol levels are followed to determine if lifestyle or drug therapy is successful. For RA, such biomarkers could be inflammatory markers or autoantibodies. Although ACPA and RF are not typically followed in individuals who have developed classifiable RA, perhaps in prevention a reduction in autoantibody level or even a reversion to levels below the cutoff value for a positive test may be strong indicators of success. In addition, as advanced imaging, such as ultrasound and magnetic resonance imaging, becomes increasingly available, these modalities may need to be considered in follow-up.
In addition to getting individuals at risk for RA to participate, for RA prevention to work on a broader level, it will be critical to have the support of a wide range of stakeholders. These stakeholders include industry, which will need to develop trials, drugs and diagnostic tools that can be used in prevention; governmental agencies, which will support the trials and infrastructure development for prevention; insurance companies; and healthcare provider systems, which will also participate in delivery of prevention. Further, the field will require a host of biomedical researchers, including clinical, translational and basic scientists, trialists, epidemiologists, public health policy experts and health economists. Digital health and social media may be an important part of publicizing, identifying, monitoring and implementing prevention.
Where Clinicians Fit In
Notably, clinicians will be a crucial part of the implementation of prevention, especially in the early stages—now—because they are likely to be the first to identify individuals who can participate in prevention studies. Individuals may have been referred to a rheumatologist because of aches, pains and ACPA positivity in the absence of clear synovitis. The temptation may exist to just treat these individuals; however, rheumatologists should be aware that RA prevention studies may be recruiting near them and that these individuals can be referred to help provide an evidence basis for RA prevention.
Further, when prevention in RA and potentially other rheumatic diseases becomes more established, clinicians will be a critical part of delivering prevention to the population. Although RA is one of the first rheumatic diseases to be evaluated for prevention, other diseases, such as lupus and gout, that follow a similar model of development of biomarker abnormalities preceding clinically apparent disease may also be targeted with preventive efforts. Indeed, an intervention trial called SMILE (Study of Anti-Malarials in Incomplete Lupus) is underway to evaluate the effectiveness of hydroxychloroquine in preventing progression of disease in people at risk for lupus.30
In sum, multiple clinical trials are now underway that may soon lead to clinically actionable, paradigm-changing ways in how we approach RA, as well as other rheumatic diseases. These clinical trials will inform the biologic changes and natural history preceding the development of RA. If successful, these trials could provide an evidence basis for pharmacologic or lifestyle interventions for patients prior to the development of clinical synovitis.
There is potential for broad implementation of RA prevention, but more work needs to be done to understand the long-term potential benefits, harms and cost effectiveness of these strategies. This model informs other rheumatic diseases that follow a similar framework of biomarker abnormalities preceding clinical onset. Rheumatologists should be aware of these advances and consider contributing to research when they are able.
 Jeffrey A. Sparks, MD, MMSc, is an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston. He uses patient-oriented and epidemiologic research studies to investigate the etiology, outcomes and public health burden of rheumatoid arthritis.
Jeffrey A. Sparks, MD, MMSc, is an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston. He uses patient-oriented and epidemiologic research studies to investigate the etiology, outcomes and public health burden of rheumatoid arthritis.
 Kevin Deane, MD, PhD, is a rheumatologist at the University of Colorado in Denver. His research interest is in the natural history of rheumatoid arthritis. He is the principal investigator on the NIH/NIAID-sponsored StopRA study, which is evaluating the role of hydroxychloroquine in the prevention of rheumatoid arthritis in individuals who are positive for antibodies to citrullinated protein antigens, but do not yet have synovitis.
Kevin Deane, MD, PhD, is a rheumatologist at the University of Colorado in Denver. His research interest is in the natural history of rheumatoid arthritis. He is the principal investigator on the NIH/NIAID-sponsored StopRA study, which is evaluating the role of hydroxychloroquine in the prevention of rheumatoid arthritis in individuals who are positive for antibodies to citrullinated protein antigens, but do not yet have synovitis.
Grant Funding/Disclosures
Drs. Sparks and Deane’s work on this manuscript was supported by NIH/NIAID Autoimmunity Center of Excellence (AI110503). Dr. Sparks is supported by NIH/NIAMS (K23 AR069688 and L30 AR066953). Dr. Deane has served as a consultant to Inova Diagnostics Inc. and Janssen Pharmaceuticals Inc. Dr. Sparks has no relevant financial disclosures.
References
- Gerlag D, Safy M, Maijer K, et al. Prevention of clinically manifest rheumatoid arthritis by B cell directed therapy in the earliest phase of the disease (PRAIRI) (abstract OP0182). Ann Rheum Dis. 2016 Jun 9. 75(Suppl 2):125.3–126.
- Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–2581.
- Deane K, Holers M, Striebich C (investigators). Strategy to prevent the onset of clinically-apparent rheumatoid arthritis (StopRA). ClinicalTrials.gov identifier NCT02603146.
- Al-Laith M (investigator). Arthritis prevention in the pre-clinical phase of RA with abatacept (APIPPRA). ISRCTN No. 46017566.
- van Schaardenburg D (investigator). Statins to prevent rheumatoid arthritis (STAPRA) prevention of rheumatoid arthritis by atorvastatin in seropositive arthralgia patients: A multicenter double-blind randomized placebo-controlled trial.
- van der Helm A (investigator). Treat early arthralgia to reverse or limit impending exacerbation to rheumatoid arthritis (TREAT EARLIER): A randomized clinical trial in recent-onset arthralgia patients that are suspect to progress to rheumatoid arthritis evaluating the efficacy of intervention with a single dose of IM corticosteroids and methotrexate.
- Rantapaa-Dahlqvist S, de Jong BA, Berglin E, Hallmans G, et al. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 2003 Oct;48(10):2741–2749.
- Nielen MM, van Schaardenburg D, Reesink HW, et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: A study of serial measurements in blood donors. Arthritis Rheum. 2004 Feb;50(2):380–386.
- Deane KD, O’Donnell CI, Hueber W, et al. The number of elevated cytokines and chemokines in preclinical seropositive rheumatoid arthritis predicts time to diagnosis in an age-dependent manner. Arthritis Rheum. 2010 Nov;62(11):3161–3172.
- Rakieh C, Nam JL, Hunt L, et al. Predicting the development of clinical arthritis in anti-CCP positive individuals with non-specific musculoskeletal symptoms: A prospective observational cohort study. Ann Rheum Dis. 2015 Sep;74(9):1659–1666.
- van de Stadt LA, Witte BI, Bos WH, van Schaardenburg D. A prediction rule for the development of arthritis in seropositive arthralgia patients. Ann Rheum Dis. 2013 Dec;72(12):1920–1926.
- Ramos-Remus C, Castillo-Ortiz JD, Aguilar-Lozano L, et al. Autoantibodies in prediction of the development of rheumatoid arthritis among healthy relatives of patients with the disease. Arthritis Rheum. 2015 Nov;67(11):2837–2844.
- Gan RW, Bemis EA, Demoruelle MK, et al. The association between omega-3 fatty acid biomarkers and inflammatory arthritis in an anti-citrullinated protein antibody positive population. Rheumatology (Oxford). 2017 Dec 1;56(12):2229–2236.
- Schett G, Emery P, Tanaka Y, et al. Tapering biologic and conventional DMARD therapy in rheumatoid arthritis: Current evidence and future directions. Ann Rheum Dis. 2016 Aug;75(8):1428–1437.
- Hemminki K, Li X, Sundquist J, Sundquist K. Familial associations of rheumatoid arthritis with autoimmune diseases and related conditions. Arthritis Rheum. 2009 Mar;60(3):661–668.
- Ferucci ED, Schumacher MC, Lanier AP, et al. Arthritis prevalence and associations in American Indian and Alaska Native people. Arthritis Rheum. 2008 Aug 15;59(8):1128–1136.
- Kolfenbach JR, Deane KD, Derber LA, et al. A prospective approach to investigating the natural history of preclinical rheumatoid arthritis (RA) using first-degree relatives of probands with RA. Arthritis Rheum. 2009 Dec 15;61(12):1735–1742.
- El-Gabalawy HS, Robinson DB, Smolik I, et al. Familial clustering of the serum cytokine profile in the relatives of rheumatoid arthritis patients. Arthritis Rheum. 2012 Jun;64(6):1720–1729.
- Hu Y, Sparks JA, Malspeis S, et al. Long-term dietary quality and risk of developing rheumatoid arthritis in women. Ann Rheum Dis. 2017 Aug;76(8):1357–1364.
- Costenbader KH, Feskanich D, Mandl LA, Karlson EW. Smoking intensity, duration, and cessation, and the risk of rheumatoid arthritis in women. Am J Med. 2006 Jun;119(6):503.e1–e9.
- Qin B, Yang M, Fu H, et al. Body mass index and the risk of rheumatoid arthritis: a systematic review and dose-response meta-analysis. Arthritis Res Ther. 2015 Mar 29;17:86.
- Di Giuseppe D, Crippa A, Orsini N, Wolk A. Fish consumption and risk of rheumatoid arthritis: A dose-response meta-analysis. Arthritis Res Ther. 2014 Sep 30;16(5):446.
- de Pablo P, Romaguera D, Fisk HL, et al. High erythrocyte levels of the n-6 polyunsaturated fatty acid linoleic acid are associated with lower risk of subsequent rheumatoid arthritis in a southern European nested case-control study. Ann Rheum Dis. 2018 Feb 7. pii: annrheumdis-2017-212274.
- Bos WH, Dijkmans BA, Boers M, et al. Effect of dexamethasone on autoantibody levels and arthritis development in patients with arthralgia: A randomised trial. Ann Rheum Dis. 2010 Mar;69(3):571–574.
- Finckh A, Escher M, Liang MH, Bansback N. Preventive treatments for rheumatoid arthritis: Issues regarding patient preferences. Curr Rheumatol Rep. 2016 Aug;18(8):51.
- Prado MG, Iversen MD, Yu Z, et al. Effectiveness of a web-based personalized rheumatoid arthritis risk tool with or without a health educator for knowledge of RA risk factors. Arthritis Care Res (Hoboken). 2018 Jan 5. [Epub ahead of print].
- Sparks JA, Iversen MD, Yu Z, et al. Disclosure of personalized rheumatoid arthritis risk using genetics, biomarkers, and lifestyle factors to motivate health behavior improvements: A randomized controlled trial. Arthritis Care Res (Hoboken). 2017 Oct 12. [Epub ahead of print].
- Tabak AG, Herder C, Rathmann W, et al. Prediabetes: a high-risk state for diabetes development. Lancet. 2012 Jun 16;379(9833):2279–2290.
- Gerlag DM, Raza K, van Baarsen LG, Brouwer E, Buckley CD, Burmester GR, et al. EULAR recommendations for terminology and research in individuals at risk of rheumatoid arthritis: Report from the Study Group for Risk Factors for Rheumatoid Arthritis. Ann Rheum Dis. 2012 May;71(5):638–641.
- Olsen N (investigator). Study of anti-malarials in incomplete lupus (SMILE). clinicaltrials.gov. NCT03030118.