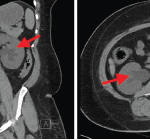
The classic distribution radiographically that favors IgG4-related RPF includes peri-aortic inflammation, typically infrarenal and extending to the iliac arteries, which sometimes entrap the ureters causing hydronephrosis.
“When [radiographic findings] are not in the classic distribution, I worry,” Dr. Stone said. “These are the cases where one can be burned.” He noted even when biopsied to rule out malignancy, the needle may go into a peri-tumoral location around a tumor where pathology can mimic IgG4-RD and miss cancer. “Only later when the patient is not responding as anticipated does it become clear it was a malignancy all along,” he said.
One tip in cases not fitting a classic radiographic distribution is to obtain biopsy to confirm histopathology and to follow patients for clinical and radiologic response. Some additional pointers of precaution are that fevers are highly atypical for IgG4-RD, so one needs to consider alternative diagnoses like malignancy (lymphoma) or Erdheim-Chester disease in patients with fever. Additionally, bulky lymphadenopathy (greater than 2 cm) is also very atypical and should be biopsied.
In Sum
This CARE session on RPF provided attendees a review of RPF including role of biopsy, important mimics in the differential not to miss, and considering RPF as an entity on the spectrum with IgG4-RD. By better characterizing RPF, hopefully this can improve diagnosis and development of future therapeutics. “I know there is a great deal of uncertainty about RPF, but I feel we are poised to make a lot of progress, finally, in this area over the next few years,” Dr. Stone said.
Mithu Maheswaranathan, MD, is an assistant professor of medicine in the Division of Rheumatology at Duke University School of Medicine in Durham, N.C.