Image Credit: Pixelbliss/shutterstock.com
One month has passed since the U.S. healthcare system overcame a historical milestone with the conversion from billing ICD-9-CM to ICD-10-CM. Although the transition to ICD-10 had a major impact on coding operations, its far-reaching tentacles go beyond coding alone and are deeply rooted in the entire revenue cycle. There is room to criticize the new codeset, but don’t be so jaded by the transition of ICD-10 to think it’s the only effect on the revenue cycle management. If we take a closer look, we see that this is something we have been struggling with since long before the introduction of ICD-10.
So what is the revenue cycle? It’s defined as, “All administrative and clinical functions that contribute to the capture, management and collection of patient service revenue.”1 Multiple functions included in the revenue cycle have to be performed at optimal levels by everyone in the practice, involving providers, managers and staff. Everyone providing patient contact should understand their role in the revenue cycle and reimbursement. Relevant areas include:
- Front end (scheduling, patient intake, registration, eligibility, benefits);
- Providers (physicians, nurses, other ancillary staff);
- Coding and billing (charge entry, coders, billers, practice managers); and
- Back end (payment posting, accounts receivable, prior authorizations, denials and appeals).
Understanding and analyzing key areas of the practice will help with resolving issues and encourage proper communication across departments to alleviate the administrative hurdles in charge capturing and revenue cycle management. Communication is a major component in shrinking any revenue leakage in the practice.
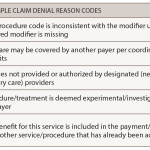
Although there are many reasons for a rejection or a denial, these lead to issues with a practice’s revenue cycle & its bottom line.
Understanding the Front End
Broad categories of the front-end role in the revenue cycle include scheduling, precertification, preregistration, patient co-pay/co-insurance and registration. The revenue cycle begins at scheduling and has a major effect on the next steps in collecting patient demographics and insurance information. Front-end staff should understand what information must be collected at scheduling for patient eligibility, medical necessity and payer-specific reimbursement policy verification as part of the process in submitting a clean claim for timely reimbursement. Because front-end staff members are not intimately involved in handling denials due to incorrect patient information, there should be a process of communicating the data in an effort to correct the problem and improve the process.
Another key area to address for front-end staff is upfront collections, because there continue to be missed opportunities to collect on patient liability. Post-insurance balances are a big component of medical practice bad debt. Front-end staff should have a clear understanding of patient responsibility for out-of-pocket expenses, co-pay and co-insurance, which should be collected at the time of service.
The Middle Man
Clinical staff play an important role in charge capturing and reconciliation, because they have the knowledge of the services rendered and are the best resource to validate the charges. Also, understanding the new code list and the documentation required by providers to be able to reach a valid code will have an impact on billing a clean claim. Clinical documentation improvement plays a vital role in ensuring that physicians have the right tools at hand to document effectively and not hold up claims in the system due to physician querying for accurate coding. It’s important to note that this is needed for the coding specificity to ensure accurate coding and minimize any rejections or denials. Practices should have a solid communication plan in place for training and educating the providers on how to document to get the most specific code and all other coding changes that will affect how claims are billed. One proactive approach in assisting providers with capturing the most accurate information is utilizing tools in the electronic medical record to give prompts or coding notes for certain diagnoses or procedures.