
I came to learn that reading poetry and reflecting about humanities made me a better person and better doctor. When I introduced medical humanities to faculty and residents on bedside rounds, they, too, became measurably better physicians and probably provided demonstrably better care. Let me explain.
How many of you carefully look at the JAMA covers and peruse the commentaries? I do. I enjoy looking at the art and reading the commentary. Sometimes I see something familiar, sometimes my skills of examination and analysis are challenged, and usually I learn something. Did anyone notice the drawing of hands on the August 25, 2010 issue of JAMA (see Figure 1)?2 As a rheumatologist, I can’t see something like that without trying to make a diagnosis. (I have one for this—what’s yours?) And did any of you happen to see the pieces about humanities and medicine in recent issues of Academic Medicine?3-5 There is more to rheumatology than rheumatology, more to medicine than medicine, and more to life than medicine.
“Inspire me with love for my art and for Thy creatures … In the sufferer let me see within only the human being … for delicate and indefinite are the bounds of the great art of caring for the lives and health of thy creatures.”
—From The Physicians’ Daily Prayer of Maimonides1

Embark on a Humanities Journey
My interest in humanities and their relationship to medicine was rekindled on one free afternoon some years ago during a meeting in Washington, D.C. I decided to visit the National Gallery of Art at the Smithsonian. I was with my daughter, Rachel, who is an artist, and my friend from our days as fellows together, Jack Caldwell (sadly, now deceased). I had taken Art 101 and 102 as an undergraduate and had some curiosity about art, and I wanted to accommodate Rachel’s wishes to tour the museum. We came upon Corot’s “Gipsy Girl with Mandolin” (see Figure 2). I was intrigued by the subject’s deformed hand. We decided to investigate possible explanations. We offered our thoughts in an essay in JAMA, which was published along with the painting on its cover.6 We suggested that this unique artistic depiction may have reflected, in some manner, the debilitating polyarticular gout that Corot was experiencing at that time in his life.
This was the beginning of a transformation of my thinking about medicine and humanities. Art, literature, and history became an enjoyable interest. Several years ago, an opportunity arose to bring this to clinical medicine in my department. Our accrediting body, the Residency Review Committee for Internal Medicine of the Accreditation Council for Graduate Medical Education, invited proposals for innovations in medical education. I was thrilled when Saint Barnabas Medical Center (where I was then medicine program director and department chair) was selected to among the 21 participating programs.
We proposed to develop and implement a humanities curriculum at the bedside. We hypothesized that such an enrichment of traditional medical education would make better people who would perform measurably better as physicians and deliver measurably better patient care. We considered that there was nothing more essential to medicine than caring, passion, empathy, compassion, and respecting our patients, all attributes of the complete physician.7-10 Although others included humanities in the curricula, we were unaware of attempts to integrate humanities into patient care or measure their effects.
Why humanities in medicine? Because, as stated by Sir William Osler, MD, “the practice of medicine is an art, based on science.” Because “the good physician treats the disease; the great physician treats the patient who has the disease.” Because they teach us to “care more particularly for the individual patient than for the special features of the disease.” Because “nothing will sustain you more than the power to recognize the true poetry of life—the poetry of the common place, of the ordinary man, of the plain toil-worn woman, with their loves and their joys, their sorrow, and their griefs.” Because the arts “secrete materials which do for society at large what the thyroid gland does for the individual. The humanities are the hormone.” Because humanities challenge us to confront existential questions of truth, knowledge, insight, purpose, and personal growth. What is life? What is our purpose? Who am I? Who are you? Who are you to me? What might I become? What is this world in which I find myself? How might it be changed for the better? How can I be a better person and physician? How can I care better for my patients? We need humanities to remind us what is truly important and why we do what we do.

We mourn that the grandeur, the glory, allure, passion, dedication, and sense of calling that once characterized medicine and enticed the best and the brightest to careers in medicine and particularly to internal medicine (and rheumatology) have faded, if not disappeared. Much has been written about the erosion of our once noble profession by external and internal factors—exigencies of time, regulatory impositions, managed care, economic incentives and disincentives, explosion of scientific knowledge, complexities of disease, an aging population, enlightened inquisitive and demanding patients and families, among other factors. It has been lamented that our traditions, values, passion, unqualified commitment, and unstinting care have eroded, and that we have lost our way if not our soul.11-18 Humanities can help restore meaning, contentment, and joy to our professional and personal lives.
Reviewing the Results
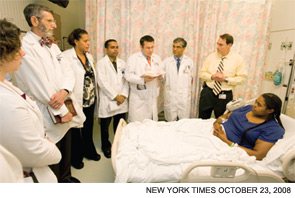
Thus we embarked on our ambitious initiative to help rediscover passionate humanism in clinical medicine. This is not the place to review our experimental design, controls, numbers, tables, graphs, and p-values, most of which have been presented elsewhere.19-22 Suffice it to say that our pilot observations, during an academic year and subsequently reproduced and extended, suggested that our bedside humanities-enriched curriculum, integrating brief, cogent, and relevant selections from humanities to daily bedside rounds (see Figure 3), measurably improved resident performance and patient care. This experience proved to be a valuable, sometimes profound, experience for the faculty and residents, indeed for the department of medicine. We changed the way the department thought about and practiced medicine. This was a very good thing.
Let my former faculty, residents, and patients briefly tell of this work in their words. You don’t always need statistics to know if you’ve affected a patient or truly touched a student or resident or colleague, to realize that an attitude and approach has changed, or to appreciate the sparkle in an eye or expression on a face. When I first told my faculty (Drs. Ashish Parikh, Sunil Sapru, Anthony Carlino, and Mindy Houng) and collaborators Dr. Paul Wangenheim and M. Martha Eide that I wanted to bring humanities to daily hospital rounds, their response was shock and disbelief. After much dialogue, education, and preparation over many months, and after initial experiences on rounds, “We slowly became believers. This became a route to learning that discussion of hypertension just doesn’t reveal. When a patient is included, it’s a particularly powerful experience, for we see them as more than the sum of their abnormal labs and radiographs. Moreover, our patients have a chance to see that we, too, are human beings.”
All were affected. “The residents and students truly enjoy our daily humanities rounds. Their journal entries reflect their personal growth, insight into human nature, and special connections with patients. There’s a tangible and measurable effect on the residents.” We came to embrace the humanities. “They keep us focused on the reason we all went into medicine in the first place—to care for that person we refer to as ‘the patient.’ We think more these days about what we do for our patients and how it affects their lives. We take more time to ask about and reflect on the unique journey of each patient. We are all better for this.”
Residents changed, too. One of my senior residents at the time, Frantz Pierre-Louis, MD, eloquently expressed the sentiments of his peers. He and his peers initially had reservations. However, he says, “as time passed, my uneasiness settled. Bedside humanities were not a burden but a precious asset that would benefit not just my career but my life in its entirety.” Indeed, he notes, “there were times when we would discuss, animatedly, issues that seemed to have nothing to do with medicine. I saw more passion in those exchanges than during traditional discussions of coronary disease.”
There were poignant experiences. “One of the best moments of my residency was encountering a patient who was a very sensitive soul in a very sick body,” Dr. Pierre-Louis describes. “She blossomed when we met with her daily to discuss a poem of her own composition. While we did not make her well, I felt so happy that we shared those delightful moments.” Although he acknowledges that “many might argue that the time it takes to do bedside humanities would be better spent taking care of patients. But what type of care for our patients are we talking about?” Dr. Pierre-Louis and his colleagues learned that, in his words, “medical humanities put everything in perspective. Each patient could be a parent, each child could be yours, and ultimately each doctor is a future patient. The good doctor needs to look at each patient with the eyes of a painter, listen to them with the ears of a musician, and analyze their emotions like a poet.”
One patient, who was introduced to a selection from the humanities curriculum to facilitate care in the ambulatory practice, said it was such a powerful moment that it brought “chills up and down my spine.”
I am enormously proud of my former residents and faculty for not just acknowledging the importance of humanistic care but for making it an essential part of the fabric of the program. We became better doctors for this, and I think our patients received better care. For example, there was the time my faculty chided me for considering the dismissal of a particularly difficult patient; they reminded me of our programmatic imperative to offer humanistic care, to continue our efforts to provide the patient-centered care we espoused, and to aspire to a higher standard. I realized then that my faculty had assimilated what I had hoped to impart about caring for patients, that they had taught me, and that they internalized values with which I still sometimes struggled, despite my idealism; indeed they had surpassed me, and that this meant that I had succeeded in our novel initiative.
Another instance was when one of our residents used his vacation to study Spanish to learn to better communicate with his patients. The candidate pool for residency began to include applicants from places that were never attracted before, presumably reflecting growing awareness of our program.
Graduates told us they were incorporating some of what we did in their practices—one was implementing a medical humanities program at his new institution. The program became affiliated with the Drew University graduate program in medical humanities and bioethics. The Healthcare Foundation of New Jersey recognized the program with their annual leadership award for humanism in healthcare. Colleagues at other medical centers contacted us about adapting the program, or they adopted what we created. We were honored that our program was featured in the November 2008 issue of the Reporter of Association of American Medical Colleges and Pauline Chen’s column in The New York Times (October 23, 2008).23,24 I truly believe these examples reflect that we changed the way our doctors think and do medicine. Humanistic medicine is now imbued in the program, is part of the lexicon, and became an identity. It has continued beyond my departure.
Final Words
What have we learned from this? Bringing humanities to the bedside is not hard. What we did can be generalized. It requires only commitment, will, and passion. It is good for doctors and patients. It may lead to better physician performance and patient care. We do not believe that classroom humanities, without translation to patient care and appropriate role modeling by physicians, imparts to others the full potential value of humanities in teaching and providing humanistic, patient-centered care. We believe that “humanities,” in the bedside setting, should be kept simple and easy for the residents and students. We believe inclusion of humanities in our professional activities, at least to some degree, is essential for us to be the best physicians we can be.
Eugene Stead, Jr., MD, who was chair at Duke where I did my residency and arguably the most influential person in American medicine in the 20th century after Sir William Osler, wrote, “take care of people, not illness … the future of medicine belongs to those … who … in spite of bureaucratic systems, pressures and financial disincentives to spend time with patients continue to care for the patients as human beings.”24,25 So does the present.
This is what we’ve tried to rediscover and bring back to medicine. I think our limited observations, but most importantly the comments and actions of my former residents and faculty, and their patients, suggest that we have. This is why I sometimes read poetry, alone and with my students, residents, colleagues, and patients. And you should, too.
Dr. Panush is professor of medicine, division of rheumatology, department of medicine, Keck School of Medicine, University of Southern California, Los Angeles.
References
- Maimonides. Oath and prayer of Maimonides. Friedenwald H, trans. Bull Johns Hopkins Hosp. 1917;28:260-261.
- Cole TB. Study of hands. JAMA. 2010;304:833.
- Muller D, Kase N. Challenging traditional premedical requirements as predictors of success in medical school: The Mount Sinai School of Medicine humanities and medicine program. Acad Med. 2010;85:1378-1383.
- Ousager J, Johannessen H. Humanities in undergraduate medical education: A literature review. Acad Med. 2010;85:988-998.
- Charon R. Commentary: Calculating the contributions of humanities to medical practice—motives, methods, and metrics. Acad Med. 2010;85:935-937.
- Panush RB, Caldwell JR, Panush RS. Corot’s ‘gout’ and a ‘gipsy girl’. JAMA. 1990;204:1136-1138.
- Panush RS. Lessons and legacies from the days of the giants. Traditions of medicine and speculation about the future. In: Panush, RS, ed. Yearbook of Rheumatology and Musculoskeletal Medicine. St. Louis/Philadelphia: Elsevier; 2006:277-307.
- Panush RS, Sergent JS. A rude awakening. JAMA. 1997;277:515-516.
- Epstein AL, Stead EA Jr, Haynes BF. A way of thinking. A primer on the art of being a doctor. Carolina Academic Press, Durham, 1995. Review. Ann Intern Med. 1996;165:351.
- Verghese A. The calling. New Engl J Med. 2005;352:1844-1877.
- Lown B. The Lost Art of Healing. Ballantine, NY: Ballantine; 1996: xiii.
- Weatherall DJ. The inhumanity of medicine: Time to stop and think. BMJ. 1994;309:1671.
- Panush RS. Upon finding a Nazi anatomy atlas: The lessons of Nazi medicine. The Pharos. 1996;59:18-22.
- Panush RS. Why I no longer accept pens (or other gifts) from industry (and why you shouldn’t either). J Rheum. 2004;31:1478-1482.
- Dittrich L. The humanities and medicine: Reports of 41 U.S., Canadian, and international programs. Acad Med. 2003;78: 951-1075.
- Coller B, Klotman P, Smith LG. Professing and living the oath: Teaching medicine as a profession. Amer J Med. 2002;112:744-748.
- Charon R, Banks JT, Connelly JE, et al. Literature and medicine: Contributions to clinical practice. Ann Intern Med. 1995;122:599-606.
- Spiro H. What is empathy and can it be taught? Ann Intern Med. 1992;116:843.
- Panush RS, Parikh A, Sapru S, et al. Read two poems and call me in the morning. Humanism for residents, health care professionals, and patients. Paper presented at: Association of Program Directors in Internal Medicine Spring Meeting; April 15-19, 2007; San Diego, CA.
- Panush RS, Parikh A, Sapru S, et al. Bedside humanities improves resident performance and patient care. Comparison of a traditional curriculum enriched with bedside humanities with a traditional educational curriculum alone. A controlled innovation. Paper presented at: Association of Program Directors in Internal Medicine Spring Meeting; April 1-3, 2008; New Orleans, LA.
- Panush RS, Parikh A, Sapru S, et al. Rx: Read two poems and call me in the morning. Bedside humanities improves resident performance and patient care. Association of Program Directors in Internal Medicine Spring Meeting; April 26-29, 2009; Dallas, TX.
- Panush RS, Parikh A, Sapru S, et al. Rx: Read two poems and call me in the morning. A medical humanities curriculum improves resident performance and patient care. II. From the hospital to ambulatory care. Association of Program Directors in Internal Medicine Spring Meeting; April 26-28, 2010; Baltimore, MD.
- Fuchs E. Humanities 101: Poetry and paintings enter the residency curriculum. Reporter of Association of American Medical Colleges. November 2008.
- Chen P. Stories in the service of making a better doctor. The New York Times. October 23, 2008.
- Stead EA. Just Say For Me. Collected by F Schoonmaker and E Metz. World Press, Denver, 1969, p 13.
- Stead EA. A Way of Thinking. A Primer on the Art of Being a Doctor. BF Haynes, ed. Carolina Academic Press, Durham, 1995. Dedication


