
Are Tendon Injections Worth a Shot?
Last month I commented about joint injections. I suggested that this may be one of those circumstances where we don’t have to be perfect, where efficacy may be just as good from injecting close to joints as in them. Along these lines, there was a nice review of whether or not injections for tendon problems are even clinically beneficial.1 The simple answer is arguably not.
For lateral epidondylitis, they were useful in the short term; data for medial epicondylitis, rotator cuff syndrome, and other tendinopathies were less impressive. It was not really surprising to me to see that the authors had difficulty finding convincing evidence for long-term benefit from steroid injections for lateral epidondylitis (and other forms of tendinous syndromes). In fact, after one year, patients with tennis elbow fared better without injections. Might steroid injections delay the recovery that would come with conservative or other therapies?
The authors’ analysis could not adduce value from tendon injections of hyaluronate, botulinum toxin, prolotherapy, platelet-rich plasma, aprotinin, or polidocanol. Are tendon injections really worth a shot?
With Complements: Plus Ça Change, Plus C’est La Même Chose
When I was a fellow (back in the “days of the giants,” when ships were iron and men were, too), there was great interest in complement. Our simplistic view of certain rheumatic diseases, exemplified by rheumatoid arthritis and some vasculitides, was of immune complex activation of complement as the explanation for tissue damage.
Early in my career as a faculty member, one of our fellows, Michel Laham, performed elegant experiments indicating that complement components perturbed mononuclear cell function.2 My colleagues and I thought this was a potentially important observation but, after Michel completed his fellowship, did not follow up on it. Certainly our understandings today invoke more intricate mechanisms focusing on cellular interactions and other mediator systems.
It was, therefore, of interest to read the report that complement activation initiated Th17 cell differentiation and expression in experimental autoimmune disease and that this may be moderated by blockade of C5aR.3 This very nice work used SKG mice that spontaneously developed arthritis that was critically dependent on Th17 cells. Activation of complement by classical, alternative, or lectin pathways triggered disease. C5a, common to the three pathways, was essential for driving Th17 cell differentiation and expression of arthritis (symptoms were suppressed in C5a-deficient animals). Co-culture experiments found that C5a acted on tissue-resident macrophages to drive Th17 differentiation. This occurred in synergy with granulocyte/macrophage colony stimulating factor or Toll-like receptor signaling. Presence of macrophages also was required for induction of arthritis. Thus extrinsic and intrinsic complement pathway activation promoted Th17 cell differentiation and expression, evoking autoimmune arthritis in these mice. Blockade of the C5a receptor may therefore be a reasonable strategy to consider in the management of these disorders.
The problem I have with studies like this is how they will translate to caring for our patients. The literature is replete with reports of successful therapeutic interventions in experimental models of rheumatic diseases that fail in humans. That, however, is why we persevere.
Stressed Out
What does social rejection have to do with inflammatory/immunologic responses? The psalmist(s) wrote of this (71:9) as have balladeers, song composers, and others. What might be the mechanism? And, might this be relevant to rheumatic disease?
Oxytocin promotes benevolence, generosity, and trust. I hadn’t known that oxytocin had a “touchy-feely” reputation, that it was perceived as an enhancer of romance, that it was used with couples counseling, that military and police were supposedly interested in its potential to change behaviors of criminals or enemies, and that it was sold on the Internet as “liquid trust.”4 However, subjects receiving the hormone before playing a game with economic consequences behaved more altruistically to members of their team and with “defensive aggression” to outsiders.5 So, oxytocin plays an interesting role in interpersonal behavior.
Another study found that social stress—impromptu speaking, publicly solving difficult math problems (those would certainly stress me!)—was associated with increases of a soluble receptor for tumor necrosis factor–α (sTNF-αRII) and interleukin 6, that brain regions which process rejection-related distress and negative affect (the dorsal anteriol cingulate cortex and anterior lingula) showed greater activity in neuroimaging, and that this correlated with elevations of sTNF-αRII.6 Thus neural responses to social threat/rejection were associated with increased inflammatory response when individuals experienced acute social stress. Might these observations suggest, at least in part, some understanding of how stress might affect our diseases?
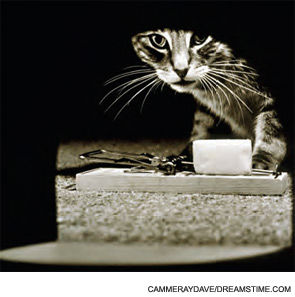
However, I’m reminded of the imaginative studies of David Trentham and colleagues from some time ago.7 They examined stress in murine collagen-induced arthritis; the stress was exposure of the mice to a cat! These experiments found that stress notably suppressed disease. These apparently conflicting observations were distressing.
From this I learn that acute and chronic stress are not good, unless you may be one of Dr. Trentham’s arthritic mice; they lead to neuro-immuno-endocrine changes which are just beginning to be examined; and oxytocin is an interesting substance with possible roles in stress and rheumatic disease. So I asked my good friend Bob Lahita, who probably knows neuro-imuuno-endocrine aspects of rheumatic diseases better than anyone, to help me put this all together. (Bob told me there is even a neuroimmunoendocrine society!)
There’s very little information about oxytocin and rheumatic disease, either as a marker of distress, a possible immunomodulator, or a mediator that might “dampen” disease expression. Oxytocin increases in response to estrogen, and is thus elevated in females, especially women stressed by disease.8 Oxytocin also increased in mycobacterial-induced arthritic rats when in extreme pain.9 Also, T-cell tolerance seemed to be modulated by oxytocin (and other neuroendocrine hormones).10-11 (Only someone like Bob would have these references.) Therefore, we would predict that oxytocin would be elevated in virtually all women with rheumatic disease. It should also be elevated in the individuals studied undergoing social stress, were it measured.
Is there a possibility certain stresses in particular circumstances could be good for patients (as they were for the mice)? Could oxytocin have played a role in the anti-arthritic effect of stress in Dr. Trentham’s mice? Could oxytocin play a role in pain in women with chronic rheumatic disease? Might this offer a possible opportunity to develop interventions? Bob will figure this out. And we will doubtless better understand the roles of stress and oxytocin on immunobiological processes in our diseases.
Dr. Panush is professor of medicine, division of rheumatology, Department of Medicine, Keck School of Medicine, University of Southern California in Los Angeles.
References
- Coombes BK, Bisset L, Vincenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: A systematic review of randomized controlled trials. Lancet. 2010;376:1751-1867.
- Laham MN, Caldwell JR, Panush RS. Modulation of human lymphocyte responses by complement. J Clin Lab Immunol. 1982;9:39-47.
- Hashimoto M, Hirota K, Yoshitomi H, et al. Complement drives Th17 cell differentialtion and triggers autoimmune arthritis. J Exp Med. 2010;207:1135-1143.
- Miller G. The prickly side of oxytocin. Science. 2010;328: 1343.
- De Dreu CKW, Greer LL, Shalvi S, et al. The neuropeptide oxytocin regulates parochial altruism in intergroup conflict among human. Science. 2010;328:1408-1411.
- Slavitch GM, Way BM, Eisenberger NI, Taylor SE. Neural sensitivity to social rejection is associated with inflammatory responses to social stress. PNAS 107, 2010 (33): 14817-14822.
- Rogers MP, Trentham DE, McCune J, et al. Effect of psychological stress on the induction of arthritis in rats. Arthritis Rheum. 1980;23:1337-1342.
- Jezová D, Juránková E, Mosnárová A, Kriska M, Skultétyová I. Neuroendocrine response during stress with relation to gender differences. Acta Neurobiol Exp. 1996;56:779-785.
- Millan MJ, Millan MH, Colpaert FC, Herz A. Chronic arthritis in the rat: Differential changes in discrete brain pools of vasopressin as compared to oxytocin. Neurosci Let. 1985;54:33-37.
- Geenen V. Thymus-dependant T-cell tolerance of neuroendocrine functions: Principles, reflections, and implications for tolerogenic/negative self-vaccination. Ann NY Acad Sci. 2006;1088:284-296.
- Geenen V, Kecha O, Brilot F, Charlet-Renard C, Martens H. The thymic repertoire of neuroendocrine-related self-antigens: The biological role in T-cell selection and pharmacological implications. Neuroimmunomodulation. 1999;6:115-125.
