Contributing Authors
- Helen Bateman, MD
- Jessica Berman, MD
- Elizabeth Brooks, MD
- Marcy B. Bolster, MD (Subcommittee Chair, 2008–2010)
- Amy Cannella, MD (Subcommittee Chair, 2010–present)
- Alan Erickson, MD
- Michelene Hearth-Holmes, MD
- Santhanam Lakshminarayanan, MD
- Deana Lazaro, MD
- Nancy Liu, MD
- Kevin McKown, MD
- Leslie Staudt, MD
- Peter Valen, MD
- Joanne Valeriano-Marcet, MD
Is there room for internal medicine (IM) housestaff to learn more about rheumatology? The ACR and its Committee on Training and Workforce Issues (COTW) assessed that there should be ample room for a broader spectrum of rheumatology teaching to IM residents. With the additional perspective of increasing rheumatology workforce needs, it also seems conceivable that if IM resident rheumatology education could be enhanced, there may be a greater demonstrated interest in pursuing fellowship training and, thus, careers in rheumatology. Notably, given increased clinical and administrative demands on rheumatology faculty coupled with either the absence of a rheumatology elective or the shortened rheumatology rotation experiences for IM residents, it seems clear that the creation of an educational tool to enhance rheumatology learning would be addressing an unmet or partially met need.
The current profile of rheumatology education for IM residents consists of a broad array of educators, including rheumatology fellows and faculty who are part of a rheumatology fellowship training program, rheumatology faculty not affiliated with a subspecialty training program, private practice rheumatologists affiliated with community IM training programs, and, less commonly perhaps, internists who are the sole teachers of rheumatology in some residency training programs. With this spectrum of rheumatology educators, the provision of a curriculum as a teaching tool could provide both structure and depth for the IM learners.
Background Research and Program Development
In 2008, the COTW Subcommittee for Resident Education performed a needs assessment for rheumatology education of all U.S. IM program directors. Of 226 surveys distributed electronically, 86 were returned (38%). The survey sought to elicit program director opinions regarding the demonstrated need for rheumatology education, ideal teaching modalities, and current methods for providing rheumatology education; space was provided for respondents to write in other ideas. Of the surveys that were returned, 42% of programs had more than 50 residents and 83% were affiliated with a rheumatology division within the department of medicine. Even more programs (94%) had at least one board-certified rheumatologist on staff. When asked who was teaching the residents, answers were nearly equally split between rheumatologists in private practice (30%), academic rheumatologists (35%), and rheumatologists affiliated with a fellowship training program (30%). Only 3% responded that rheumatology was taught solely by internists.
Of the respondents, 94% believed that a formal curriculum would be beneficial, and specific requests were made for interactive web-based modalities. The avoidance of another DVD tool was specifically requested! It was clear from the survey results that an interactive online teaching tool, utilizing a case-based learning approach, would be well received. Additionally, a competency-based approach to learning rheumatology would meet the needs for IM resident education as well as IM program director curriculum development.
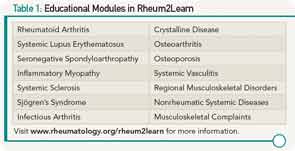
The COTW Subcommittee for Resident Education included 13 members, predominantly, though not entirely, composed of rheumatology fellowship program directors, who convened twice yearly and by conference call on an ad hoc basis to draft the essential learning modules (2008–2012). Initially described as the “Sweet Sixteen,” the essential topics were selected to provide formatted rheumatology education to IM housestaff, and were later narrowed to a core of fourteen interactive, web-based learning modules (see Table 1), entitled Rheum2Learn (www.rheumatology.org/rheum2learn). Each of the modules encompasses two cases on the specified learning topic; one case is a more straightforward diagnostic clinical presentation, followed by a second case that presents a clinical scenario of higher complexity with more advanced facets of clinical management. At the end of each case, the author for each module has posed several questions, accompanied by a discussion of the case and answers to these queries.
The remainder of each module is composed of learning objectives categorized within each of the six Accreditation Council for Graduate Medical Education core competencies (medical knowledge, patient care, interpersonal communication, professionalism, practice-based learning and improvement, and systems-based practice). The learning objectives use Bloom’s taxonomy and provide embedded links to internet-based learning tools.1 Examples include images from the ACR Rheumatology Image Bank, Internet-based modalities such as a video demonstration of the musculoskeletal examination, a link to the National Osteoporosis Foundation education pages on bone health, published classification criteria, and many PubMed articles pertinent to the selected topic discussion.
Quantifying Program Benefits
Rheum2Learn provides IM housestaff with plenty of room for learning rheumatology over the course of IM training. Having been available online since November 2012, Rheum2Learn is gaining greater general recognition by word of mouth. It will be shared with the attendees of the upcoming national meeting of the Association of Program Directors of Internal Medicine. It is equally important that rheumatologists who are involved in IM resident education publicize this freely available product to IM program directors.
Many roles for this tool have been suggested, ranging from delivering a self-study tool for IM housestaff to providing a structure for a guided tutorial led by rheumatology faculty or fellows in a small-group learning environment. The hope is that Rheum2Learn can provide a platform for teaching IM residents during the short exposure they have while rotating on a rheumatology elective, and it can be implemented outside of the rheumatology rotation to provide a useful resource throughout the remainder of the IM training period. Importantly, it will be valuable to track the use of the tool and to develop a method for assessing outcomes from its implementation. One such outcome measure might include IM resident performance on the medicine in-service examination.
Rheumatologists have a narrow window of time during which to expose IM house staff to the evaluation of the patient with rheumatic disease, including demonstrating the key portions of the history, the nuances of the physical exam, the breadth of the differential diagnosis, the efficient use of resources to evaluate the differential diagnostic considerations, and the selection of medications, with awareness demonstrated of potential adverse effects. Lack of study time during a rheumatology elective, or even exposure to a rheumatologist during a three-year IM residency, can make learning rheumatology during a single specified period challenging. Thus, the provision of a structured and interactive tool, easily accessible for self-study or more formalized teaching, should enhance rheumatology learning during IM residency training.
Increased education in training will have many obvious positive results. We recognize the shortfalls of the rheumatology workforce, the needs for recruitment of more capable physicians into our field, and the link of possible solutions to our needs with improved IM residency education in rheumatology. In addition to the goal of increasing the passion for internists seeking subspecialty training, we hope to fill the room to learn more rheumatology!
Dr. Bolster is associate physician and director of the rheumatology fellowship training program at Massachusetts General Hospital in Boston.