
WavebreakMedia / offset
“Don’t believe everything you think,” said Allan Lokos, the founder and guiding teacher of the Community Meditation Center located in New York City’s upper west side. These words may be especially important for those dealing with chronic pain, finds new multicenter research.
The study, “Trajectories of Fear-Avoidance Beliefs on Physical Activity Over Two Years in People with Rheumatoid Arthritis,” appeared in the May 2018 issue of Arthritis Care & Research.1 Researchers from Sweden and the U.S. set out to explore the relationship between beliefs about pain and physical activity in patients with rheumatoid arthritis (RA), a topic that, to date, has had limited attention in the literature.
The researchers enrolled 2,569 RA patients (77% women, mean age 58 years), all of whom completed the Fear-Avoidance Beliefs Questionnaire physical activity subscale (FABQ-PA). Principal investigator Christina H. Opava, PhD, RPT, is director of Strategic Research Area Health Care Science and chair of Doctoral School in Health Care Sciences at the Karolinska Institutet in Sweden. With patients recruited from the Swedish Rheumatology Quality registers, the investigators set out to shed light on patients with differing trajectories of fear-avoidance beliefs over two years and predictors for each trajectory.
Dr. Opava states, “For 40 years I have been researching the importance of psychosocial factors for physical activity. My colleagues and I wanted to better understand why, despite the achievement of better inflammation control via medications, there remain many RA patients who report significant levels of pain and fatigue. Specifically, we wanted to examine what leads many of these patients to avoid physical activity.”

Dr. Opava
Dr. Opava says, “We looked at changing patterns in this large sample and ended up with a diagram where each line represents one patient, and they cluster together in certain ways. So if you group them according to clusters, then you get trajectories. We chose a three-trajectory solution that makes sense, both clinically and statistically. Included were four items from the FABQ-PA on beliefs about physical activity causing pain and injury: 1) pain is caused by physical activity, 2) physical activity makes one’s pain worse, 3) physical activity might be harmful, and 4) one should not do physical activity that might worsen one’s pain.
“The scale went from 0 (do not agree at all) to 6 (agree); values over 15 have been shown to indicate high fear avoidance. Three trajectories of fear-avoidance beliefs were identified: low (mean FABQ-PA=3), moderate (mean FABQ-PA=9) and high (mean FABQ-PA=15).”
More Fear Than Expected
“It was quite a surprise,” says Dr. Opava, “to find that one out of five patients with RA displayed high fear-avoidance beliefs because there is no reason for them to believe that exercise will do them harm or cause more pain. When most patients have an injury or inflammation they experience pain, confront it and recover. Those who catastrophize, however, have more pain-related fear, and avoid chores and physical activity. Then it becomes a vicious cycle—they don’t use their bodies, they experience more pain, followed by more fear, etc.
“Two other predictors of the high fear-avoidance trajectory were low income and low education level,” she continues. “It is a well-known fact that these affect all kinds of poor health behaviors and beliefs. For example, if you have pain or inflammation, then your natural reaction is to rest to avoid the pain and inflammation. That is a reasonable reaction if it’s acute pain, but with RA, the pain is chronic and will only increase if you completely refrain from physical activity.
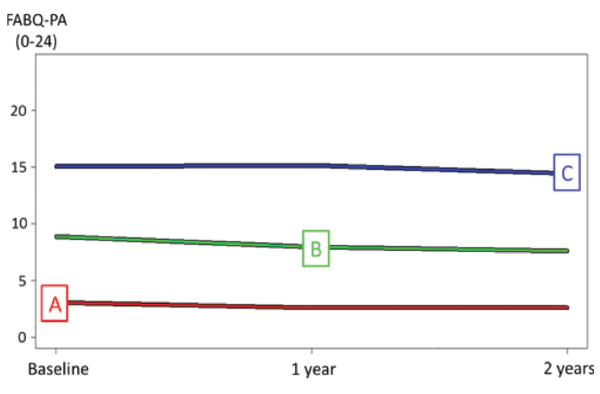
Figure 1: Trajectories of Fear-Avoidance Beliefs on Physical Activity Over Two Years in People with RA
Three trajectories of fear-avoidance beliefs identified by K-means cluster analysis: A=low (41% of the total sample), B=moderate (41% of the total sample) and C=high (18% of the total sample). Total sample N=2,569. Values indicate the average over a two-year period. FABQ-PA=Fear-Avoidance Beliefs Questionnaire physical activity subscale.
“In general, it is easier for educated people to find health information online, and indeed they may find it easier to trust people ‘like them’ who are educated [the health professionals]. If you have poor health literacy, then you are prone to believe in erroneous ‘facts’ that you hear from friends and elsewhere (don’t move, rest the knee, use hot packs). And if you accept this advice, then you may be less interested in evidence-based information.
“Interestingly, we found that men were more likely to hold fear-avoidance beliefs and to be in the trajectory with high fear-avoidance beliefs. This is a bit controversial, but we have reason to believe that despite Sweden supposedly being a country where the sexes are equal, women still do the majority of the daily chores. Thus, women need to confront pain whether they feel like it or not. … They have to keep going no matter what. Men are most often the primary breadwinner, but they can take time off from work and use the national insurance so they are in bed or resting quite a bit.”
A gradual exposure process can be used to acclimatize patients to physical activity, so they learn how to move in a safe way under the proper guidance.
The Power of Words, Perception
“One thing that can affect pain catastrophizing is threatening or frightening illness information,” states Dr. Opava. “While some health professionals do advise patients in pain to avoid physical activity, it is not likely that they would admit this. Frankly, it seems that many healthcare providers are not saying ‘avoid activity’ outright. … It’s just that they are unconsciously sending signals to take it easy and rest a lot when in pain.
“And if healthcare providers are telling patients that physical activity doesn’t harm their joints or increase pain—and if they are not accustomed to exercising—then they are probably not going to start.”
Dr. Opava offers the following advice:
- The message to move should initially come from the physician or nurse, but if further counseling is necessary then a physical therapist can be brought in to more fully explain things; and
- A gradual exposure process can be used to acclimatize patients to physical activity, so they learn how to move in a safe way under the proper guidance.
She says, “This process is frequently used with patients experiencing low back pain. In patients with RA, however, it is not used systematically because it has long been considered that pain is strongly related to inflammation, and thus, if you exercise, you increase the inflammation activity—but that is not the case in the majority of patients. We actually have data suggesting that exercise reduces pain and inflammation.”
Counseling Patients
It can be challenging to act as part physician, part psychologist, but given the results of this study, it might be a bit easier. Regarding how to counsel patients, Dr. Opava says, “Ask, for example, ‘Are you afraid of moving because you are concerned that your knee or arthritis will worsen?’ If the answer is ‘yes,’ then try to convey that the information you are giving them is evidence based. And if the next time you see the patient, she or he is not active, then have them meet with a physical therapist. In addition, we have found that it helps if a health professional works with the patient to set SMART [specific, measurable, attainable, relevant, and timely] goals. You can, for example, have them agree to take a walk around the block and then, when that goal is reached, set a new higher goal.
“Given our findings, we now have a better idea of how to target our resources. Patients need information that can help calm them down, help them understand the signals that their bodies are giving off, arrest the catastrophic thinking and get them moving.”
Elizabeth Hofheinz, MPH, MEd, is a freelance medical editor and writer based in the greater New Orleans area.
Reference
- Demmelmaier, I, Björk, A, Dufour, AB, et al. Trajectories of fear-avoidance beliefs on physical activity over two years in people with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2018 May;70(5):695–702.



