Rheumatologists have growing concerns about how we manage rheumatoid arthritis (RA) and the disease outcomes we are achieving.1 Over the past two years, clinician rheumatologists have begun working together to address these problems through the Rheumatoid Arthritis Practice Performance (RAPP) Project, a nationwide clinical quality-improvement initiative. The RAPP Project has now grown to 168 participants managing more than 80,000 RA patients. We will describe the problems RAPP clinicians have identified within our current RA management and highlight several high-impact improvements we are testing and implementing.
Disease Registry
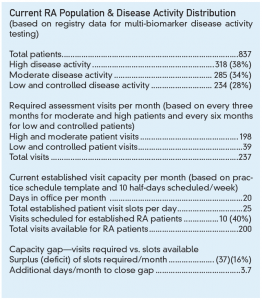
When the RAPP Project initially asked its participants how many RA patients they manage, what percentages of their RA population have active disease or controlled disease and what percentage are overdue for intended office visits, they had no answers. When they then began using a simple disease registry to manage their RA populations as part of this quality-improvement project, most identified many more RA patients than they had imagined. They also learned that the frequencies of their assessments for patients with controlled, low, moderate and high disease activity fell far short of those recommended by the Treat-to-Target Task Force, the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR).2-4 Evidence of these disease assessment gaps was presented at the 2014 ACR/ARHP Annual Meeting (see Figure 1).5,6

(Click for larger image)
Figure 1: Multi-biomarker assessment data from the aggregated populations of 44 RAPP Project rheumatology practices: Unassessed and overdue patients.
Treat-to-Target RA Management under Current Practice Models
The population management registries of RAPP Project participants have documented that assessing RA disease activity during physician office visits creates an unmanageable workload. We not only lack the visit capacity to see, assess and manage our RA patient populations at the recommended frequencies, but we are also unable to consistently do all the necessary work ourselves for individual patients during these scheduled visits.
Consider the evidence. RAPP Project practices have, on average, 585 RA patients per rheumatologist full-time equivalent (range 67–1,800), representing about 40% of the established patients seen in a typical week.5 Practices with mid-level providers predictably manage more patients per rheumatologist, but experience similar visit capacity issues.
The Treat-to-Target Task Force recommends assessing patients with moderate and high disease activity monthly, and those with controlled and low disease activity every three to six months.2 Many RAPP clinicians feel it’s appropriate to perform assessments at intervals of three months for patients with moderate or high disease activity and six months for those with controlled or low disease activity, allowing that some patients will be scheduled more or less frequently as their needs require. Yet even with these more lenient disease assessment frequencies, our median percentage overdue for the moderate and high cohort is 66% and for the controlled and low cohort is 52%.6 Moreover, these percentages overdue remain stable from month to month within individual practices, despite RAPP physicians fully intending to perform assessments at every scheduled visit and having access to lists of overdue patients from our registries.