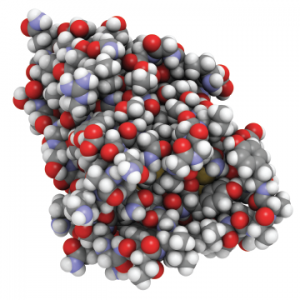
An all-atom representation of nanobodies—small antibodies found in camels, dromedaries and llamas.
molekuul_be / shutterstock.com
MADRID—The anti-IL6 “nanobody,” vobarilizumab, produced mixed results when used with methotrexate (MTX) and compared with MTX and placebo, according to results of a 24-week, double-blind Phase 2b study of patients with rheumatoid arthritis (RA), which were presented in an abstract session at the Annual European Congress of Rheumatology (EULAR).
The drug missed its primary endpoint in producing an ACR20 response at Week 12 compared with placebo, but produced sustained remissions among patients in the three highest dosing groups, said Thomas Dorner, MD, professor of rheumatology and clinical immunology at Charite University Hospitals in Berlin.
The session covered new findings on biologic therapies for RA, also touching on initial efficacy findings on the immunocytokine, dekavil, and an analysis of cancer risk for patients on biologics.
Nanobodies, developed by the vobarilizumab study sponsor, Belgium-based Ablynx, are heavy-chain-only antibodies derived from camelids—camels, llamas and other animals. The company hails them as “ideal building blocks” for new biological therapies, because they have full binding capacity, with a smaller, more stable structure.
In the study, 345 patients who’d had an insufficient response to MTX were randomized to receive placebo and MTX or one of four doses of vobarilizumab plus MTX—75 mg every four weeks, 150 mg every four weeks, 150 mg every two weeks or 225 mg every two weeks.1
Patients were forced to discontinue the drug if there was less than 20% improvement in both swollen and tender joints at Weeks 12, 16 and 20. Patients could not have been on a disease-modifying anti-rheumatic drug (DMARD) in the previous four weeks or on a biological DMARD or JAK inhibitor in the previous six months, and only 13% had had any previous exposure to a biological DMARD or JAK inhibitor.
There was no significant difference in ACR20 response between the study groups as a whole and the placebo group by Week 12.
But significantly more patients in the three highest treatment groups achieved DAS28 CRP scores of less than 2.6 and low disease activity after Weeks 12 and 24 than those in the placebo group (P<.01), Dr. Dorner said.
Researchers also found that about a third of patients in the three highest treatment groups had a sustained ACR50 response from Week 12 through Week 24. And sustained remission defined by DAS28CRP of less than 2.6 at Weeks 12, 16, 20 and 24 was seen in 20–25% of the patients in the three highest dosing groups, compared with 3% in the placebo group, they found.

