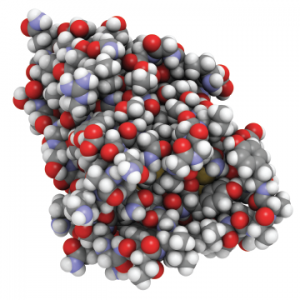
An all-atom representation of nanobodies—small antibodies found in camels, dromedaries and llamas.
molekuul_be / shutterstock.com
MADRID—The anti-IL6 “nanobody,” vobarilizumab, produced mixed results when used with methotrexate (MTX) and compared with MTX and placebo, according to results of a 24-week, double-blind Phase 2b study of patients with rheumatoid arthritis (RA), which were presented in an abstract session at the Annual European Congress of Rheumatology (EULAR).
The drug missed its primary endpoint in producing an ACR20 response at Week 12 compared with placebo, but produced sustained remissions among patients in the three highest dosing groups, said Thomas Dorner, MD, professor of rheumatology and clinical immunology at Charite University Hospitals in Berlin.
The session covered new findings on biologic therapies for RA, also touching on initial efficacy findings on the immunocytokine, dekavil, and an analysis of cancer risk for patients on biologics.
Nanobodies, developed by the vobarilizumab study sponsor, Belgium-based Ablynx, are heavy-chain-only antibodies derived from camelids—camels, llamas and other animals. The company hails them as “ideal building blocks” for new biological therapies, because they have full binding capacity, with a smaller, more stable structure.
In the study, 345 patients who’d had an insufficient response to MTX were randomized to receive placebo and MTX or one of four doses of vobarilizumab plus MTX—75 mg every four weeks, 150 mg every four weeks, 150 mg every two weeks or 225 mg every two weeks.1
Patients were forced to discontinue the drug if there was less than 20% improvement in both swollen and tender joints at Weeks 12, 16 and 20. Patients could not have been on a disease-modifying anti-rheumatic drug (DMARD) in the previous four weeks or on a biological DMARD or JAK inhibitor in the previous six months, and only 13% had had any previous exposure to a biological DMARD or JAK inhibitor.
There was no significant difference in ACR20 response between the study groups as a whole and the placebo group by Week 12.
But significantly more patients in the three highest treatment groups achieved DAS28 CRP scores of less than 2.6 and low disease activity after Weeks 12 and 24 than those in the placebo group (P<.01), Dr. Dorner said.
Researchers also found that about a third of patients in the three highest treatment groups had a sustained ACR50 response from Week 12 through Week 24. And sustained remission defined by DAS28CRP of less than 2.6 at Weeks 12, 16, 20 and 24 was seen in 20–25% of the patients in the three highest dosing groups, compared with 3% in the placebo group, they found.
Dr. Dorner attributed the discrepancy between the lack of ACR20 response and the sustained remission rates to the forced discontinuation at Week 12 and what may have been an inflated placebo response, because so many of the patients had very limited access to biologic therapy and a chance to receive open-label extension therapy after the actual study period.
“The results overall are indicative for a strong potential for disease-modifying activity of vobarilizumab, supporting treat-to-target management of RA,” Dr. Dorner said.
In the Crosshairs
In another study, the fully human immunocytokine, dekavil, demonstrated good initial safety and efficacy results in Phase 1b. Immunocytokines involve fusing an antibody and a cytokine—in this case, the vascular-targeting antibody F8 fused to IL10—for what is intended to be better targeting of disease, ideally sparing normal tissue.2
RA patients, who had not responded to at least one TNF inhibitor, were treated with one of 10 doses—6 µg/kg to 600 µg/kg—along with a fixed MTX dose, said Mauro Galeazzi, MD, professor of rheumatology at the University of Siena in Italy.
Just one of 35 patients had a dose-limiting toxicity or serious adverse event. That patient, in the 450 µg/kg group, experienced grade 2 purpura and grade 2 dyspnea, which was not deemed drug related, and fully recovered after one week of being treated with corticosteroids.
After eight weeks, improvement was seen in ACR or EULAR response criteria, or both, in 62.5% of the 24 patients able to be evaluated. Two patients, at 30 µg/kg and 60 µg/kg, had an ACR70 response for more than a year after their treatment ended, Dr. Galeazzi said.
The drug is now being studied in Phase 2, at 30 µg/kg and 160 µg/kg, with MTX. “We have already included in the study 23 patients, and we are waiting for 45 patients to give you the interim analysis,” he said.
A third study examined a large Swedish database and found no significant increase for first solid or hematologic cancer risk among RA patients taking tocilizumab, abatacept, rituximab or a TNF inhibitor for the first time, compared with those taking conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs). There was also no increased risk for those on a second TNF inhibitor.3
The study, by researchers at Karolinska Institute in Stockholm, was an analysis of data from linked national and population Swedish registers and included more than 63,000 patients—1,693 tocilizumab patients, 1,894 abatacept patients, 3,119 rituximab patients, 10,300 on a first TNF inhibitor and 4,130 on a second TNF inhibitor, with 42,365 patients on csDMARDs as a reference group. Patients with previous malignancies were excluded, and researchers didn’t include non-melanoma skin cancers in their overall analysis. Researchers adjusted for age, sex, comorbidities, hospital stays, use of non-steroidal anti-inflammatory drugs and other factors.
Researchers did find one significantly increased risk: Squamous cell skin cancer among patients treated with abatacept had a hazard ratio of 2.2 compared with those on csDMARDs.
But Hjalmar Wadstrom, a PhD student at Karolinska who presented the study, said this finding “should be interpreted cautiously” and that it could be “simply due to multiple testing.” But he added it shouldn’t be “just disregarded and needs to be further studied.”
“This study confirms previous findings of no increased risk of overall cancer with TNF-inhibitor treatment, neither as a first nor a second biologic,” he said, “Also, for tocilizumab, abatacept and rituximab, this study showed no increased risk of overall cancer.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Dorner T, Weinblatt, M, Durez P, et al. Remission and maintenance of efficacy in a phase 2b study of vobarilizumab, an anti-interleukin 6 receptor nanobody, in patients with moderate-to-severe rheumatoid arthritis despite treatment with methotrexate (abstract OP0098). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.
- Galeazzi M, Sebastiani G, Voll R, et al. Safety, tolerability and initial signs of efficacy of the fully human immunocytokine dekavil (F8IL10): A novel therapeutic approach for rheumatoid arthritis (abstract OP0099). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.
- Wadstrom H, Frisell T, Askling J. Overall cancer risk in patients with rheumatoid arthritis treated with TNF inhibitors, tocilizumab, abatacept, or rituximab (abstract OP0100). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.

