megaflopp/shutterstock.com
SAN FRANCISCO—“We’ve known for a long time that prescription medications and illicit drugs can both mimic and actually induce the autoimmune syndromes treated by rheumatologists,” Jonathan Graf, MD, professor of medicine at the University of California–San Francisco in the Division of Rheumatology at Zuckerberg San Francisco General Hospital (SFGH), said at the California Rheumatology Alliance 2016 Scientific & Medical Meeting in May.
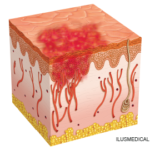
“There are syndromes associated with drug use that look like their non-drug counterparts, but with particular calling-card features,” Dr. Graf explained in a follow-up interview with The Rheumatologist. The worst of these is vasculitis. “It’s important for rheumatologists to have a generalized understanding of the drugs their patients may take, legal or not, that [have an] impact on autoimmune diseases. For many of these syndromes, you have an obvious treatment—get the patient to stop taking the drug and the condition may abate.” Unfortunately, there is little evidence to support medical treatments for some of these drug-related syndromes, he said, although skin grafts, antibiotics and systemic corticosteroids have been tried.
Detective Work
In his presentation, Dr. Graf described some detective work done by the rheumatologists at SFGH on a sequence of eight patients admitted to the hospital in 2009, starting with a 46-year-old woman who presented with cyanosis in her lower extremities. These patients presented a distinct syndrome with a puzzling mix of clinical manifestations including necrotic retiform purpura on the face and ears, skin necrosis, vasculopathy, neutropenia and acute kidney injury, along with characteristic autoantibody profiles and other laboratory findings. “The syndrome we were seeing had features that were not classic vasculitis. We realized there was a common thread, which was cocaine use, but not the classic syndrome of that.”
After a thorough investigation, it turned out they all were using cocaine that had been adulterated with levamisole, an anti-parasitic agent used in veterinary medicine and once a treatment for rheumatoid arthritis until it was discontinued in 1990 due to side effects. An advisory from the federal Substance Abuse and Mental Health Services Administration around the same time reported that 70% of the cocaine tested in July 2009 by the Drug Enforcement Administration was positive for levamisole.1 Since then, levamisole adulteration has been on the rise, although the full extent of the syndrome is not fully appreciated.
This relatively new phenomenon is just the tip of the iceberg when it comes to rheumatologic disorders secondary to drug use, Dr. Graf said. “We’ve been called in with patients to rule out vasculitis. I’m now getting called in to see every weird cocaine toxicity in the hospital.” The rheumatologist often sees disease patterns for which the cause is unknown—or else genetically linked. In cases where features associated with drug use are present, it would be good to do a work-up for drug use, including a thorough medication history and, in some cases, urine drug screening. “Ask your patients about their drug use.”
Some patients with substance use disorders may find it difficult to stop taking the drug that triggered their rheumatologic disorder, Dr. Graf acknowledged. And some patients using drugs like cocaine may not fit the stereotypical profile of a drug user. “Even with someone you wouldn’t expect to be using these drugs, it’s a mistake to assume that it’s not a concern. In fact, cocaine use is prevalent in all aspects of society.” An estimated 1.9 million Americans actively used the illegal drug in 2008.
‘It’s important for rheumatologists to have a generalized understanding of the drugs their patients may take, legal or not, that [have an] impact on autoimmune diseases.’ —Dr. Graf
Varieties of Drug Manifestations
There are many ways that cocaine can trigger inflammatory responses. These include blood vessel diseases, vasoconstriction and cocaine-associated midline destructive lesions that start with chronic sinusitis and mimic granulomatosis with polyangiitis, as well as a host of garden variety rheumatologic disorders and reports of more unusual types of cocaine-associated vasculitis. “Cocaine is associated with well-described autoimmune disorders,” Dr. Graf said. Treatment is based on recognizing the disease and encouraging cessation of cocaine use. There is also some case report-level evidence for using high-dose methylprednisolone.
Less well described are rheumatologic disorders directly linked with heroin, but these include membranoproliferative glomerulonephritis, other renal diseases and amyloidosis. Other vascular syndromes are associated with methamphetamines, MDMA (ecstasy), ADHD medications, such as Adderall and Ritalin, and other prescription medications. Even over-the-counter cold preparations, such as pseudoephedrine, can induce vasculopathy. Other examples include drug-induced lupus, hydralazine-induced vasculitis, pulmonary hypertension and necrotizing glomerulonephritis.
“We see a lot of things that don’t exactly fit the typical disease. You have to ask yourself: Is something else going on?” Dr. Graf said. “We often don’t know, but these patients may be losing tolerance to multiple antibodies and antigens,” he adds. For the front-line rheumatologist, urine toxicology screening can detect cocaine metabolites for up to 72 hours, but won’t detect levamisole, for which LC Tandem mass spectrometry is needed. Another tool for the doctor is to screen for anti-neutrophil cytoplasmic antibodies with fluorescence imaging.
Larry Beresford is an Oakland, Calif.-based freelance medical journalist.
Reference
- SAMHSA. Nationwide public health alert issued concerning life-threatening risk posed by cocaine laced with veterinary anti-parasite drug. Press Release. 2009 Sep 21. http://www.samhsa.gov/newsroom/press-announcements/200909210445.