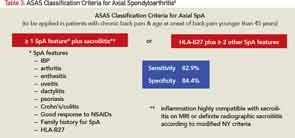
The ASAS classification criteria require the patient have chronic low back pain (i.e., longer than three months’ duration) starting before the age of 45 years and either the presence of sacroiliitis on imaging (i.e., X-ray or MRI scan) with one typical feature of spondyloarthritis or the presence of HLA-B27 and two features of spondyloarthritis6 (see Table 3).
The obvious advantage of these criteria is to help recognize the nonradiographic forms of the disease so the rheumatologist can initiate early treatment. Although the sensitivity and specificity of these criteria are quoted to be 83% and 84% respectively, inappropriate application of the classification criteria for diagnostic purposes—especially in the absence of any objective signs of inflammation—in clinical practice may lead to errors. It’s imperative to understand that although the same clinical features included in the classification criteria are used in making the diagnosis, in practice, one first needs to rule out other common conditions that may cause similar symptoms. In addition, one needs to take into consideration the pretest probability of axSpA. Checking boxes of the classification criteria set would indeed lead to inaccurate conclusions.
With tumor necrosis factor-α inhibitors (TNFi) showing promise in large trials on nr-axSpA patients, such erroneous diagnosis may lead to inappropriate treatment with expensive and potentially harmful medication. The question of how to avoid this over-diagnosis and inappropriate treatment was central during the discussions held at a recent Federal Drug Administration (FDA) advisory committee meeting and led to the denial of approval for both adalimumab and certolizumab for the treatment of nr-axSpA patients. This FDA denial means that there is no approved medication to treat nr-axSpA in the U.S. and has led to new questions:
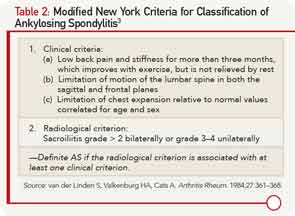
What should the regulatory pathway be for approval of new agents for nr-axSpA? How can we prevent the unintended use of the classification criteria for diagnostic purposes? Do we need new diagnostic criteria for axial spondyloarthritis? Has the time come to update the Modified New York Criteria that were developed 30 years ago in the pre-MRI era?
MRI’s Role
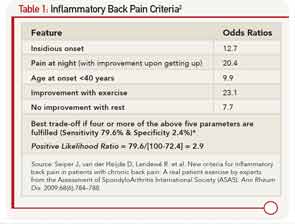
What is the appropriate role of MRI of the sacroiliac joints and HLA-B27 in daily practice for establishing the diagnosis of axial spondyloarthritis? In the era of prudent use of healthcare dollars, it’s important to order expensive investigations only as a part of a thoughtful protocol for diagnostic evaluation. A patient with chronic low back pain (i.e., lasting for three months or longer) starting before the age of 45 has a 5% chance of having axSpA.7 Before ordering expensive investigations, a careful history (including past history and family history) and detailed physical examination may reveal signs and symptoms of spondyloarthritis and would increase these odds dramatically. The presence of inflammatory back pain on history would increase the odds of axial spondyloarthritis to 14%, and an additional one or two SpA features would increase the odds to 35–70%, respectively.7 In this situation, the presence of HLA-B27 or X-ray changes of sacroiliitis should clinch the diagnosis of axSpA or AS respectively.