Specialty pharmacy utilizers
Source: CVS Health Enterprise Analytics
Presenters at the Access in Rheumatology meeting held in advance of the ACR’s State-of-the-Art Clinical Symposium took a deep dive into the access challenges faced by rheumatology patients and discussed possible solutions.
Treatment
At least until 2026, prescription drug spending will exceed the U.S. gross domestic product (GDP) and health spending, said rheumatologist Colin C. Edgerton, MD, American Rheumatology Network, Charleston, S.C. Much of that spending is attributed to the purchase of specialty drugs, including those prescribed by rheumatologists.
High drug prices and recent drug shortages, such as for hydroxychloroquine and methotrexate, are among the healthcare access challenges rheumatology patients face. One example Dr. Edgerton discussed was a 100% increase in the price of adalimumab over the past five years. The trends of higher drug prices and shortages lead to prescription abandonment and lack of adherence, he said.
High drug costs have led to an increase in prior authorization requirements, with one American Medical Association survey cited by Dr. Edgerton showing two hours of physician paperwork spent for every hour of direct patient care. “It’s a leading source of physician dissatisfaction,” he said.
Dr. Edgerton outlined the growth of value-based medicine that focuses on higher quality and lower costs, even for some rheumatology drugs and shared barriers that rheumatologists often face when tracking outcomes, due to smaller practice sizes and the financials involved with tracking analytics.
Specialty Drug Prices

Dr. Chaguturu
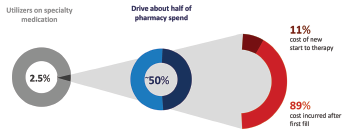
Sree Chaguturu, MD, chief medical officer for CVS Caremark, offered a perspective on the role of pharmacy benefit managers and shared more data on the high costs involved with specialty drugs. One example: Specialty medications are used by only 2.5% of the total population, but account for about 50% of the total drug spending. The majority of those costs are incurred by those who continue on therapy rather than newer users, he explained.
The use of specialty medications will only increase going forward. Of 537 drugs in the drug pipeline over the next three years, 355 are specialty drugs. There also are 283 existing drugs that will have new specialty indications, Dr. Chaguturu said. “This is fantastic for new opportunities to manage comorbidities and patient conditions, but sponsors want to make sure there is appropriate access and pricing.”
Gene therapy and hyperinflation are adding to costly therapies, but biosimilars are mitigating these by creating competition and potentially lowering costs, Dr. Chaguturu said.
The entry of biosimilars to the market has been slow in the U.S. compared to Europe, but will eventually assist with cost savings, Dr. Edgerton said.
Determining a Fair Price

Ms. Emond
According to Sarah Emond, MPP, executive vice president and COO of the Institute for Clinical and Economic Review in Boston, healthcare providers and their patients don’t have to choose between affordability and access. “We have to acknowledge the reality, but there is another path. If we acknowledge that, we can talk about fair prices leading to fair access and plenty of revenue to help with the innovation we want,” she said.
Even if drugs are priced fairly, patients may not get access to newer therapies because the price is still high, said Ms. Emond.
The nonprofit Institute for Clinical and Economic Review has completed value assessments to ensure the price paid for a drug matches the benefits a patient is receiving. This involves looking at obvious health benefits, such as living longer, but also components that can be harder to measure, such as ethical priorities and benefits beyond price. “It’s important to talk about the value of those,” Ms. Emond said.
‘[Obtaining prior authorization] is a leading source of physician dissatisfaction.’ —Dr. Edgerton
Within rheumatoid arthritis, one option is the use of novel, broad access, pay-up-to formulas that would allow patients more access to drugs and cause fewer utilization management hurdles. “Using our calculation of fair price across conditions like rheumatoid arthritis, you set a maximum price and let patients have access to the care they need,” she said.
Ms. Emond is encouraged by pricing principles recently introduced by Novartis and Sanofi, including transparency and limited U.S. increases, that would push the concept of fairer drug prices to the forefront (https://tinyurl.com/uxyzkj6w and https://tinyurl.com/uzdx4m6h).
Get Involved
The Access in Rheumatology session wrapped up with ways that rheumatologists can get involved from a legislative perspective to help improve access to care and give the specialty of rheumatology a stronger voice. Marcus Snow, MD, assistant professor of internal medicine, Division of Rheumatology, University of Nebraska, Omaha; and Elizabeth (Blair) Solow, MD, assistant professor of medicine, Division of Rheumatic Diseases, UT Southwestern, Dallas, shared their suggestions. Dr. Solow is chair of the ACR’s Government Affairs Committee, and Dr. Snow is chair of the ACR’s Committee on Rheumatologic Care.
Although physicians may feel siloed when providing care, they actually are in touch with a wide range of stakeholders in the healthcare system, including pharmacy benefit managers, nursing staff and many others, Dr. Solow said. “We should be at the table helping make health policy decisions federally and at the state level that impact rheumatology providers.”
Here are ways to get involved and help continue to improve access to care:
- Attend conferences and sessions that discuss legislative issues;
- Use the ACR’s Legislative Action Center and the Voter Voice app to contact lawmakers. The ACR has prepopulated letters on such issues as step therapy and student loan repayment. You can add a line to share a personal note about a patient or explain how something related to these issues has affected your practice, Dr. Solow said;
- Stay up to date on key policy issues with resources like ACR@Work, an e-newsletter deployed twice a month;
- Contribute to RheumPAC, the ACR’s nonpartisan political action committee. “This is a way members can use funds to be at meetings with legislators who are working on issues impacting rheumatology,” Dr. Solow said;
- Take part in the ACR’s visits to Capitol Hill that are scheduled twice a year. You don’t need “expert knowledge” of policy issues to attend, Dr. Solow said. You only need passion to share your experience as a healthcare provider with lawmakers.
“The ACR will help walk you through where the issues stand and what we believe. I never felt unprepared,” Dr. Snow said.
Dr. Solow updated attendees on some of the bills that affect rheumatology, including two bills (H.R. 2163 and S. 464) related to step therapy that have good traction in both the House and Senate, with bipartisan support. “We’re hoping to get those across the finish line or attached to other large pieces of legislation,” she said.
There also is a bill for prior authorization that has not been introduced yet in the 117th Congress.
Vanessa Caceres is a medical writer in Bradenton, Fla.



