An extensive infection workup was negative.
(click for larger image)
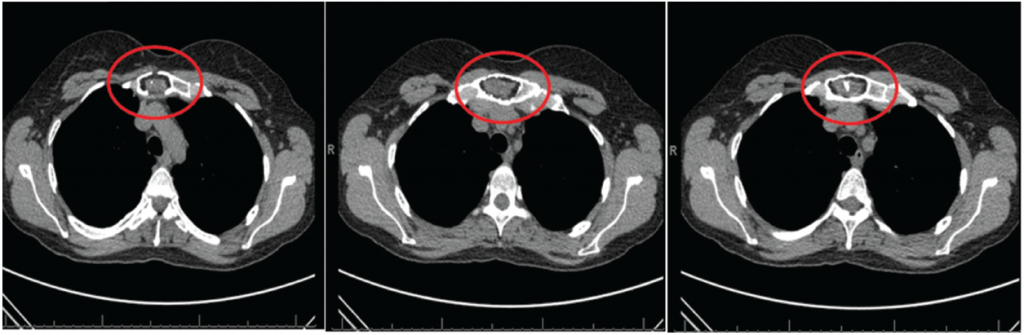
Figure 1: CT scan of the chest with three sagittal sections revealing no evidence of interstitial lung disease or air trapping. Focal lytic lesion in the manubrium (circle) with cortical destruction/defect and internal soft tissue component.
Her chest radiograph revealed no infiltrates. X-ray of the sacroiliac joints revealed bilateral sacroiliitis. Chest CT scan revealed mild apical scarring with minimal bibasilar dependent atelectasis with no evidence of interstitial lung disease or air trapping. A focal-lytic lesion in the manubrium with cortical destruction/defect and internal soft-tissue component was reported.
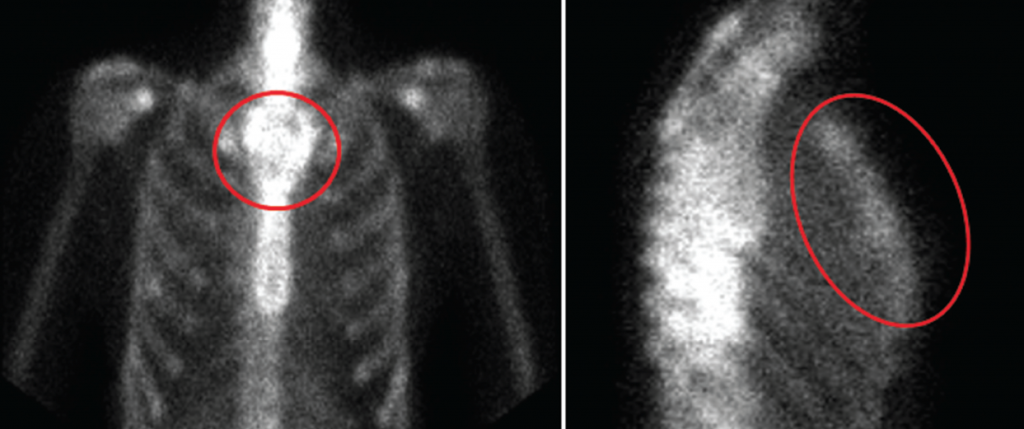
The findings were concerning for a more aggressive lesion-like plasmacytoma (see Figure 1). A whole-body bone scan was recommended and revealed an irregular, expanded appearance of the manubrium, which correlated with the lytic lesion seen on chest CT, with no foci of increased radiotracer activity to suggest osseous metastatic disease (see Figure 2).
(click for larger image)
Figure 2: Whole-body bone scan revealing irregular, expanded appearance of the manubrium, which correlates with the lytic lesion seen on recent chest CT with no foci of increased radiotracer activity to suggest osseous metastatic disease.
An open incisional biopsy of the manubrium revealed a pathological picture diagnostic for chondromyxoid fibroma, which was confirmed by three pathologists from different institutions (see Figures 3 and 4).
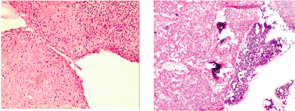
Figure 3 (left): Low-power view with extensive myxomatous and chondroid areas with condensation of the stromal cells (H&E).
Figure 4 (right): Low-power view with bone marrow surrounding extensive myxomatous and chondroid areas with condensation of the stromal cells (H&E).
Case Summary
The patient has a history of hypertension and hypothyroidism and presented with clinical features suggestive of an overlap connective tissue disease, with clinical manifestations of scleroderma, ankylosing spondylitis and lupus-like symptoms.
Differential Diagnosis
In the context of the history and physical exam, systemic sclerosis was high on the differential given the following manifestations: constitutional symptoms, sclerodactyly distal to the MCP, Raynaud’s, GERD, fine crackles on physical exam, nail fold changes on capillaroscopy and high titer-positive IF-ANA with speckled pattern and elevated inflammatory markers.
According to 2013 ACR/EULAR classification criteria for diagnosing scleroderma, she fulfilled 15 points, which indicates a definitive diagnosis of scleroderma.
Sjögren’s syndrome was listed in the differential in the context of sicca symptoms, lung involvement and positive SSA/SSB titers, which can be isolated or associated with other autoimmune diseases, such as SLE.

