A 47-year-old Caucasian woman presented to the rheumatology clinic with a one-year history of pain and swelling involving the wrists, hands, ankles and feet that progressively worsened. Her symptoms included generalized fatigue, morning stiffness in the hands and lower back lasting more than an hour, Raynaud’s phenomena (triphasic), photosensitivity, tightening of the skin of the hands and feet, heartburn, chest wall tenderness, exertional dyspnea, sicca symptoms and an unintentional weight loss of 30 lbs. over the prior six months.
She had previously been evaluated by another rheumatologist for a four-year history of lower back pain associated with stiffness, which was relieved by non-steroidal anti-inflammatory medications (NSAIDs) and activity. Imaging of the sacroiliac joints revealed bilateral sacroiliitis, and she was diagnosed with ankylosing spondylitis.
One year before, she was also given the diagnosis of scleroderma, due to symmetrical skin thickening distal to the MCPs, synovitis of her MCP and PIP joints, the presence of Raynaud’s phenomenon and a history of esophageal reflux symptoms. She was treated with prednisone 20 mg daily and hydroxychloroquine 200 mg twice daily with minimal improvement in her symptoms.
Medical History
Her medical history was remarkable for hypertension, hypothyroidism and right carpal tunnel release. She was up to date on risk- and age-appropriate malignancy screenings, including mammogram, pap smears and vaccinations.
Social & Family History
The patient was born and raised in Michigan and is happily married with two healthy children. She is employed and is a nonsmoker. She denies chronic alcoholism or illicit drug use. There is no family history of an autoimmune disease.
Physical Examination
At the time of presentation, she was in no acute distress, with a blood pressure of 156/97 mmHg, pulse of 82 beats/min, oxygen saturation of 97% on room air, afebrile and a BMI of 22.9 kg/m2.
Her physical exam was remarkable for synovitis involving the metacarpophalangeal joints bilaterally, sclerodactyly distal to the MCPs bilaterally, dusky bluish cold extremities with no ulcerations, chest wall tenderness at the costovertebral junction and over the manubrium, diffuse bilateral inspiratory fine crackles, tenderness in the gluteal region bilaterally and a positive Patrick’s test. Nail fold capillaroscopy revealed altered capillary distribution. No facial telangiectasias were noted.
Laboratory Evaluation
Laboratory workup revealed a normocytic anemia with a hemoglobin of 10.9, MCV 90, ESR 65, CRP 2.6, positive IF-ANA (1:1280 speckled), RNP titer of 159, SSA 135, SSB 74, positive anti-centromere antibodies and a positive HLA-B27. Chemistry panel, urine analysis, RF, CCP, anti-Smith antibodies, C3, C4, anti-dsDNA, anti-phospholipid antibodies and ANCA titers were within normal ranges.
An extensive infection workup was negative.
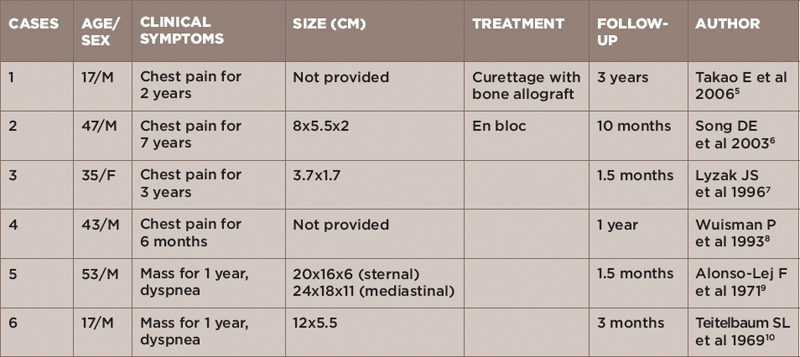
(click for larger image)
Figure 1: CT scan of the chest with three sagittal sections revealing no evidence of interstitial lung disease or air trapping. Focal lytic lesion in the manubrium (circle) with cortical destruction/defect and internal soft tissue component.
Her chest radiograph revealed no infiltrates. X-ray of the sacroiliac joints revealed bilateral sacroiliitis. Chest CT scan revealed mild apical scarring with minimal bibasilar dependent atelectasis with no evidence of interstitial lung disease or air trapping. A focal-lytic lesion in the manubrium with cortical destruction/defect and internal soft-tissue component was reported.
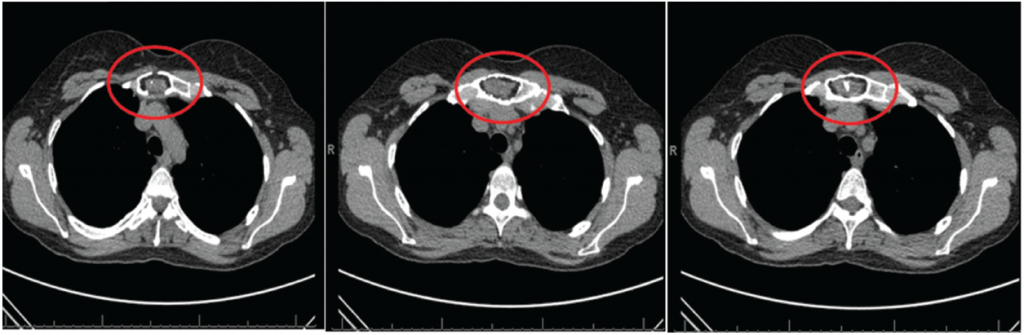
The findings were concerning for a more aggressive lesion-like plasmacytoma (see Figure 1). A whole-body bone scan was recommended and revealed an irregular, expanded appearance of the manubrium, which correlated with the lytic lesion seen on chest CT, with no foci of increased radiotracer activity to suggest osseous metastatic disease (see Figure 2).
(click for larger image)
Figure 2: Whole-body bone scan revealing irregular, expanded appearance of the manubrium, which correlates with the lytic lesion seen on recent chest CT with no foci of increased radiotracer activity to suggest osseous metastatic disease.
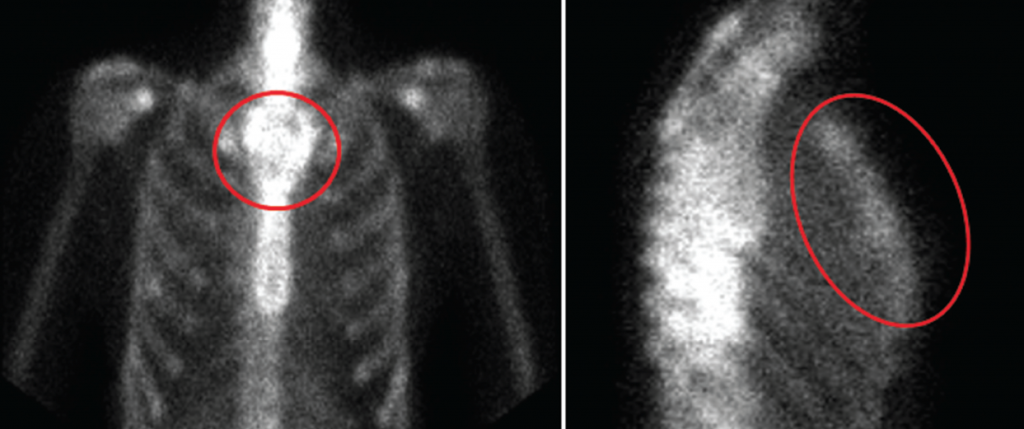
An open incisional biopsy of the manubrium revealed a pathological picture diagnostic for chondromyxoid fibroma, which was confirmed by three pathologists from different institutions (see Figures 3 and 4).
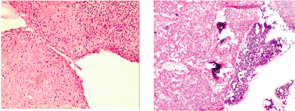
Figure 3 (left): Low-power view with extensive myxomatous and chondroid areas with condensation of the stromal cells (H&E).
Figure 4 (right): Low-power view with bone marrow surrounding extensive myxomatous and chondroid areas with condensation of the stromal cells (H&E).
Case Summary
The patient has a history of hypertension and hypothyroidism and presented with clinical features suggestive of an overlap connective tissue disease, with clinical manifestations of scleroderma, ankylosing spondylitis and lupus-like symptoms.
Differential Diagnosis
In the context of the history and physical exam, systemic sclerosis was high on the differential given the following manifestations: constitutional symptoms, sclerodactyly distal to the MCP, Raynaud’s, GERD, fine crackles on physical exam, nail fold changes on capillaroscopy and high titer-positive IF-ANA with speckled pattern and elevated inflammatory markers.
According to 2013 ACR/EULAR classification criteria for diagnosing scleroderma, she fulfilled 15 points, which indicates a definitive diagnosis of scleroderma.
Sjögren’s syndrome was listed in the differential in the context of sicca symptoms, lung involvement and positive SSA/SSB titers, which can be isolated or associated with other autoimmune diseases, such as SLE.
The back pain is suggestive of an underlying inflammatory condition, such as seronegative spondyloarthropathy, likely ankylosing spondylitis.
Could she be experiencing an autoimmune storm resulting in manifestations of different autoimmune disease and resulting in a malignancy? Mammograms and pap smears testing were normal. She had not yet undegone colonoscopy.
Discussion
Our patient had a biopsy-proved diagnosis of chondromyxoid fibroma (CMF) of the manubrium, presenting with clinical manifestations of scleroderma, ankylosing spondylitis and lupus-like features. To our knowledge, this is the first reportable case of CMF presenting with overlap syndrome.
CMF is a benign neoplasm accounting for less than 1% of all bone tumors. It has a predilection for men in the second and third decades of life with the metaphyseal regions of the long bones of the lower extremities as the favored sites of occurrence. Other sites include the small bones of the feet and the ilium.1
Radiographically, CMF manifests as an eccentrically situated, well-circumscribed, oval metaphyseal lesion parallel to the long axis of the bone. On MRI, depending on the varying amounts of myxoid and cartilage tissue, the center of the tumor is hyperintense on T2-weighted spin-echo images and short inversion time inversion recovery sequences. The typical aspects of chondroid, fibrous and myxoid tissues are not present in each histological specimen. Therefore, a small biopsy could lead to a false-negative diagnosis.
The tissue manifestations, areas with large numbers of cells with loose connective tissue stroma penetrated by lobulated areas of chondroid material with increased numbers of cell nuclei at the periphery of the chondroid lobules with plump hyperchromatic nuclei, are characteristic of CMF. Treatment in most of the reported cases consists of intralesional curettage. Excision with or without bone grafting is often performed.2
Association between antecedent autoimmune diseases and malignancy has been reported in autoimmune diseases, such as systemic lupus erythematosus, dermatomyositis and rheumatoid arthritis, systemic sclerosis and Sjögren’s syndrome. Patients with malignancies may develop autoimmune and rheumatic manifestations by induction of autoimmunity characterized by the generation of autoantibodies against a wide range of autoantigens.3 Sera of patients with malignancies were found to bind antinuclear autoantibodies, DNA, histones, Ro, La, Sm and RNP.4
Patient’s Course
The patient underwent excision of the tumor with bone grafting.
Final Diagnosis
Primary chondromyxoid fibroma of the sternum is quite rare, with only six cases documented in the literature (see Table 1). To our knowledge, this is the first reportable case of CMP presenting with undifferentiated connective tissue.
 Rajaie Namas, MD, is a clinical lecturer in rheumatology and a member of the Department of Internal Medicine, Division of Rheumatology, University of Michigan, Ann Arbor, Mich.
Rajaie Namas, MD, is a clinical lecturer in rheumatology and a member of the Department of Internal Medicine, Division of Rheumatology, University of Michigan, Ann Arbor, Mich.
 Reshma Khan, MD, is a clinical rheumatologist at Family Arthritis Center, in private practice in Palm Beach, Fla.
Reshma Khan, MD, is a clinical rheumatologist at Family Arthritis Center, in private practice in Palm Beach, Fla.
 Bernard Rubin, DO, MPH, is head of the Division of Rheumatology at Henry Ford Hospital, Detroit, Mich., where both Drs. Namas and Khan were fellows.
Bernard Rubin, DO, MPH, is head of the Division of Rheumatology at Henry Ford Hospital, Detroit, Mich., where both Drs. Namas and Khan were fellows.
Disclosure
Dr. Namas is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases under grant number T32AR007080-37.
Acknowledgments
To the patient who gave us the trust to manage her medical condition.
References
- Dahlins UK. Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed Philadelphia, PA: Lippincott-Raven. 1996;59–69.
- Wu CT, Inwards CY, O’Laughlin S, et al. Chondromyxoid fibroma of bone: A clinicopathologic review of 278 cases. Hum Pathol. 1998 May;29(5):438–446.
- Durr HR, Lienemann A, Nerlich A, et al. Chondromyxoid fibroma of bone. Arch Orthop Trauma Surg. 2000;120(1–2):42–47.
- Abu-Shakra M, Buskila D, Ehrenfeld M, et al. Cancer and autoimmunity: Autoimmune and rheumatic features in patients with malignancies. Ann Rheum Dis. 2001 May;60(5):433–441.
- Takao E, Morioka H, Yabe H, et al. Chondromyxoid fibroma of the sternum. J Thorac Cardiovasc Surg. 2006 Aug;132(2):430–431.
- Song DE, Khang SK, Cho KJ, Kim DK. Chondromyxoid fibroma of the sternum. Ann Thorac Surg. 2003 Jun;75(6):1948–1950.
- Lyzak JS, Gurley J, Boyle C, et al. Chondromyxoid fibroma of the sternum. Skeletal Radiol. 1996 Jul;25(5):489–492.
- Wuisman P, Scheld H, Tjan T, et al. Chondromyxoid fibroma of the sternum. Case report. Arch Orthop Trauma Surg. 1993;112(5):255–256.
- Alonso-Lej F, De Linera FA. Resection of the entire sternum and replacement with acrylic resin. Report of a case of giant chondromyxoid fibroma. J Thorac Cardiovasc Surg. 1971 Aug;62(2):271–280.
- Teitelbaum SL, Bessone L. Resection of a large chondromyxoid fibroma of the sternum: Report of the first case and review of the literature. J Thorac Cardiovasc Surg. 1969 Mar;57(3):333–340.