A diagnosis of right-sided DVT was made on the grounds of history, physical examination and POCUS.
The patient was admitted to the inpatient medical service for anticoagulation and further workup. During hospitalization, whole-leg ultrasonography confirmed POCUS findings, and a CT angiogram of her chest later revealed a saddle pulmonary embolus. She had no hemodynamic compromise, and echocardiography showed no right heart strain and an ejection fraction of 55%. Oral contraceptives were discontinued, and she was discharged on rivaroxaban.
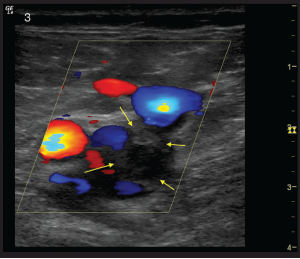
Figure 3: A transverse view of the right common femoral and saphenous junction again visualized with Color Flow Doppler mode. Flow is present in the common femoral artery and saphenous vein. A clot in the common femoral vein (outlined by yellow arrows) can be seen as a filling defect with flow seen around the clot.
She was later readmitted for worsening right lower extremity pain and swelling, and repeat whole-leg ultrasound showed clot propagation despite use of rivaroxaban.
Thrombolysis was performed, and a postprocedure extremity ultrasound revealed clearance of DVT. A CT of the abdomen and pelvis was ordered and was negative for malignancy or venous compression. Anti-cardiolipin and beta-2-glycoprotein antibodies were negative, but she was found to be heterozygous for prothrombin G20210A (Factor II mutation). Anticoagulation was changed to enoxaparin at discharge.
Unfortunately, a second recurrence of DVT occurred despite compliance with enoxaparin. Her care was also complicated by MSSA bacteremia with septic thromboembolism. The bacteremia caused an interruption in the use of etanercept, and her joint pains worsened. The joint pain persisted even after etanercept was restarted. An academic thrombosis center was consulted and recommended dual anticoagulation with enoxaparin and warfarin, and she was scheduled to follow-up there for further evaluation.
The thrombosis center hematologist evaluated her and ordered a rheumatoid factor that was 5,330 IU/mL (reference range
In follow-up with rheumatology, the patient’s prednisone dose was increased and methotrexate transitioned from oral to subcutaneous; etanercept and hydroxychloroquine were continued. Her joint pain improved on this regimen.
She remains on dual anticoagulation and continues to follow up with hematology.
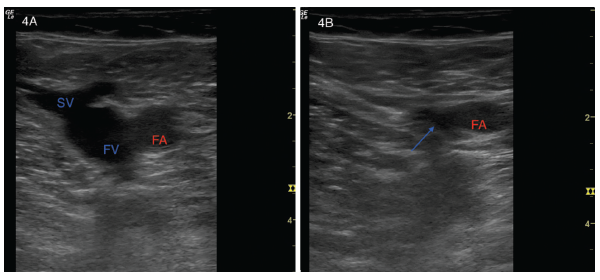
Figures 4A and B: (Left) A transverse view of a normal left common femoral artery (FA), left common femoral vein (FV) and left saphenous vein (SV). (Right) Light compression collapses the saphenous vein, and the blue arrow points to the collapsed region of the left common femoral vein. The femoral artery (FA) remains patent.
Discussion
Venous thromboembolism (VTE), including pulmonary embolism and DVT, is an important problem for general medical patients, and there is some evidence to suggest that inflammatory conditions, specifically RA, convey an independent risk factor for VTE.1