Case
A 46-year-old Caucasian female presented to the outpatient rheumatology clinic where she had been followed for several years. Her chief complaint was pain in her right knee, posterior right thigh and right hip that had begun gradually over the previous three weeks.
Her past medical history was significant for rheumatoid arthritis (RA), obesity and fibromyalgia, and she was compliant with her regimen of methotrexate, low-dose prednisone, hydroxychloroquine and etanercept. She was also taking an oral contraceptive.
She reported that the knee pain began after she performed some repairs on her automobile. One week prior to the rheumatology appointment, she saw an outside physician who believed she was experiencing an RA flare and prescribed a prednisone taper, without benefit. The knee pain progressed to include the right hip and posterior thigh, and she noticed swelling of the right lower extremity in the days prior to the appointment. She denied any trauma, recent travel or exposures. She reported a family history of unprovoked deep vein thrombosis (DVT) and pulmonary embolism in her mother that occurred at age 70. She denied a history of tobacco use.
Vital sign measurements were unremarkable, without fever, tachycardia or tachypnea. On physical examination, there was no evidence of synovitis in her upper extremity joints. The right lower extremity was mildly edematous compared with the left lower extremity. Warmth was noted unilaterally on the right lower extremity. Flexion and external rotation of the right hip joint elicited pain. No erythema, trauma or rash was noted on either extremity.
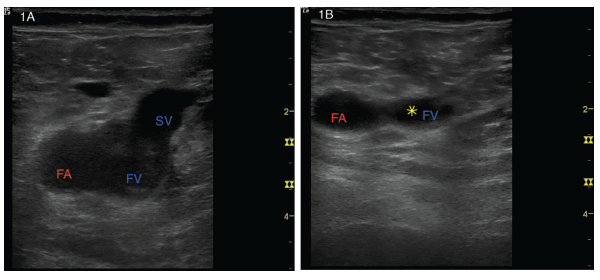
Figures 1A and B: (Left) A transverse view of the right common femoral artery (FA), right common femoral vein (FV) and right saphenous vein (SV). (Right) With gentle probe pressure, the saphenous vein collapses easily, but the common femoral vein is noncompressible. The yellow star represents the clot preventing collapse.
Due to concern for DVT, a two-region point-of-care ultrasound (POCUS) protocol was performed in the rheumatology clinic to scan for DVT of the right lower extremity. Lack of complete compressibility of the right femoral vein at the saphenous junction (see Figures 1A and B, above right) and the popliteal vein (see Figures 2A and B) was noted with intraluminal clot visualized. Color Flow Doppler was applied at the saphenous junction with disruption of flow due to the clot (see Figure 3). The left deep veins were fully compressible (see Figures 4A and B).
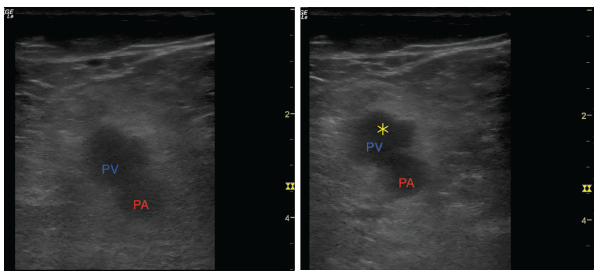
Figures 2A and B: (Left) A transverse view of the popliteal artery (PA) and popliteal vein (PV). (Right) Light compression with transducer shows an inability to collapse the popliteal vein. The yellow star represents the clot preventing collapse.
A diagnosis of right-sided DVT was made on the grounds of history, physical examination and POCUS.
The patient was admitted to the inpatient medical service for anticoagulation and further workup. During hospitalization, whole-leg ultrasonography confirmed POCUS findings, and a CT angiogram of her chest later revealed a saddle pulmonary embolus. She had no hemodynamic compromise, and echocardiography showed no right heart strain and an ejection fraction of 55%. Oral contraceptives were discontinued, and she was discharged on rivaroxaban.
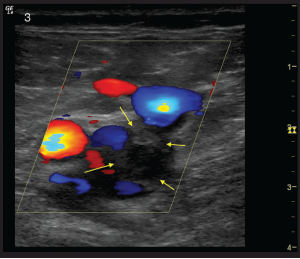
Figure 3: A transverse view of the right common femoral and saphenous junction again visualized with Color Flow Doppler mode. Flow is present in the common femoral artery and saphenous vein. A clot in the common femoral vein (outlined by yellow arrows) can be seen as a filling defect with flow seen around the clot.
She was later readmitted for worsening right lower extremity pain and swelling, and repeat whole-leg ultrasound showed clot propagation despite use of rivaroxaban.
Thrombolysis was performed, and a postprocedure extremity ultrasound revealed clearance of DVT. A CT of the abdomen and pelvis was ordered and was negative for malignancy or venous compression. Anti-cardiolipin and beta-2-glycoprotein antibodies were negative, but she was found to be heterozygous for prothrombin G20210A (Factor II mutation). Anticoagulation was changed to enoxaparin at discharge.
Unfortunately, a second recurrence of DVT occurred despite compliance with enoxaparin. Her care was also complicated by MSSA bacteremia with septic thromboembolism. The bacteremia caused an interruption in the use of etanercept, and her joint pains worsened. The joint pain persisted even after etanercept was restarted. An academic thrombosis center was consulted and recommended dual anticoagulation with enoxaparin and warfarin, and she was scheduled to follow-up there for further evaluation.
The thrombosis center hematologist evaluated her and ordered a rheumatoid factor that was 5,330 IU/mL (reference range
In follow-up with rheumatology, the patient’s prednisone dose was increased and methotrexate transitioned from oral to subcutaneous; etanercept and hydroxychloroquine were continued. Her joint pain improved on this regimen.
She remains on dual anticoagulation and continues to follow up with hematology.
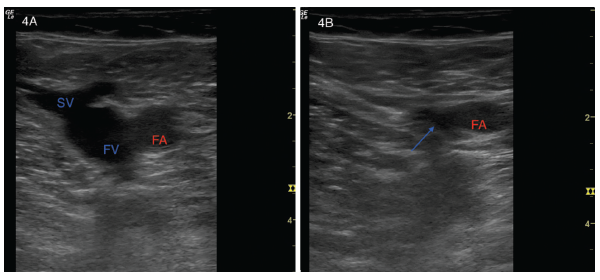
Figures 4A and B: (Left) A transverse view of a normal left common femoral artery (FA), left common femoral vein (FV) and left saphenous vein (SV). (Right) Light compression collapses the saphenous vein, and the blue arrow points to the collapsed region of the left common femoral vein. The femoral artery (FA) remains patent.
Discussion
Venous thromboembolism (VTE), including pulmonary embolism and DVT, is an important problem for general medical patients, and there is some evidence to suggest that inflammatory conditions, specifically RA, convey an independent risk factor for VTE.1
Regardless of the influence of RA on the VTE in the case above, several other risk factors should be noted, including obesity, oral contraceptive use, family history of VTE and prothrombin gene mutation. Her complicated course would have been difficult to predict upon initial evaluation by rheumatology, but the use of POCUS expedited her care.
As performed above, POCUS for diagnosis of DVT using two-region compression has been shown to be an accurate, reproducible and quickly learned method to detect DVT. In one large study, a limited two-region ultrasound paired with D-dimer strategy was shown to be equivalent to whole-leg ultrasonography for the management of symptomatic patients with suspected DVT.2
Ultrasound use has increased in rheumatology fellowships over the past decade, but has been predominantly limited to musculoskeletal ultrasound (MSUS). A recent survey was sent to various postgraduate training programs to determine the trends in MSUS training in the U.S.3 Formal MSUS training programs were present in 90% of rheumatology fellowships that responded to the survey, and various methods of training were employed, such as didactic lectures, scanning sessions with models or cadavers, interventional sessions and Web-based modules. The program directors surveyed believed that MSUS training was an important aspect of fellowship. Certifications in MSUS exist to further training, and many rheumatologists obtain these and use MSUS frequently in practice.
Although rheumatologists can be thought of as specialists in the study of disorders of the musculoskeletal (MSK) system, many of the diseases seen have extra-articular manifestations that require a multisystem approach to care. MSUS has shown utility in the practice of rheumatology; however, expansion with additional POCUS modalities is feasible.
In the above case, a POCUS DVT scan was performed in the rheumatology clinic. Although the risk of VTE associated with RA can be argued, the clinical scenario of a DVT may be common enough to warrant the addition of this skill by rheumatologists. More established extra-articular manifestations of RA, such as pericardial effusion, congestive heart failure, pleural effusion and even interstitial lung disease (ILD) can also be diagnosed and monitored with POCUS in the ambulatory setting.4
Preliminary studies suggest that physicians with limited training in lung ultrasound using pocket-sized devices can attain a high sensitivity for ILD in RA patients. If confirmed in larger trials, this may lead to reductions in CT scanning for early detection of ILD in this population.
As ultrasound machines have become more portable and affordable, there has been a dramatic increase in ultrasound education among medical schools in recent years, and integrated ultrasound curricula have been developed across the four years of medical school.5 The ultrasound topics covered include bedside echocardiography, vascular, abdominal, lung, MSK, FAST examination and RUSH protocol, among others. Medical students who complete the curriculum rate it as an important component of their education and useful for future practice.
Increasing numbers of students and residents are graduating from programs with ultrasound curricula, and they will begin fellowship in rheumatology with established skills in POCUS to supplement their MSUS training. As leaders in MSUS, rheumatology fellowships are strongly positioned to integrate additional modalities of POCUS that show utility in diagnosis and monitoring of the broad extra-articular manifestations of rheumatic diseases.
 Alvin Lee Day, MD, is in his third year of postgraduate education in the Department of Internal Medicine, Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C. He will begin a rheumatology fellowship at the University of Alabama at Birmingham this year.
Alvin Lee Day, MD, is in his third year of postgraduate education in the Department of Internal Medicine, Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C. He will begin a rheumatology fellowship at the University of Alabama at Birmingham this year.
 James W. Fant Jr., MD, is an associate professor of clinical internal medicine, and director of the Division of Rheumatology, Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C.
James W. Fant Jr., MD, is an associate professor of clinical internal medicine, and director of the Division of Rheumatology, Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C.
 Michael Wagner, MD, FACP, RDMS, is an assistant professor of clinical internal medicine and director of internal medicine ultrasound education at Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C.
Michael Wagner, MD, FACP, RDMS, is an assistant professor of clinical internal medicine and director of internal medicine ultrasound education at Palmetto Health/University of South Carolina School of Medicine, Columbia, S.C.
References
- Ungprasert P, Srivali N, I, et al. Risk of venous thromboembolism in patients with rheumatoid arthritis: A systematic review and meta-analysis. Clin Rheumatol. 2014 Mar;33(3):297–304.
- Bernardi E, Camporese G, Büller HR, et al. Serial 2-point ultrasonography plus D-dimer vs whole-leg color-coded Doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis: A randomized controlled trial. JAMA. 2008 Oct 8;300(14):1653–1659.
- Berko NS, Goldberg-Stein S, Thornhill BA, Koenigsberg M. Survey of current trends in postgraduate musculoskeletal ultrasound education in the United States. Skeletal Radiol. 2016 Apr;45(4):475–482.
- Cogliati C, Antivalle M, Torzillo D, et al. Standard and pocket-size lung ultrasound devices can detect interstitial lung disease in rheumatoid arthritis patients. Rheumatology (Oxford). 2014 Aug;53(8):1497–1503.
- Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curricular (iUSC) for medical students: 9-year experience. Crit Ultrasound J. 2015 Dec;7(1):18.