Systemic capillary leak syndrome (SCLS) is a very rare disorder, characterized by recurrent episodes of severe hypotension, hypoalbuminemia and hemoconcentration.1 Attacks of SCLS occur in three phases: 1) prodrome; 2) hypovolemia with weight gain; and 3) hypervolemia with fluid overload and polyuria often complicated by pulmonary edema. Often, compartment syndrome can lead to rhabdomyolysis as a serious complication of SCLS.2
As of 2010, 126 cases of SCLS had been reported worldwide, and few cases have been reported since that time.3 No previous literature describes a case of SCLS in a patient with prior rheumatoid arthritis (RA).
Case Presentation
A 58-year-old man with past medical history of RA, gastrointestinal (GI) upset and asthma presented at the emergency department of George Washington Hospital at midnight one summer night in 2014 with severe nausea, vomiting and diffuse abdominal pain and bloating. He denied fever and diarrhea. He reported that he had experienced gastrointestinal upset for two or three days prior to his admission, but his full admitting symptoms had been present only since 6 p.m. the day before.
In 2009, the patient was diagnosed with RA (positive RF and negative cyclic citrullinated peptide). He first presented with hand pain. He was initially treated with methotrexate, but it was discontinued in July 2011 due to GI upset. The patient was then treated with leflunomide, which he was still using daily at time of admission.
In the emergency department, he was noted to have stable blood pressure of 112/74 and a pulse rate of 130. He received intravenous fluids, pain medications and anti-emetics. He had a CT scan of the abdomen notable for a possible early/partial small bowel obstruction.
While in the emergency department, his labs were notable for a white blood cell count of 14.92, hemoglobin 19.9, hematocrit 58.7 and platelet 353. His creatinine was 1.7, albumin 5.2, bicarbonate 17.2, anion gap 30 and lactate 4.3. (See Table 1)
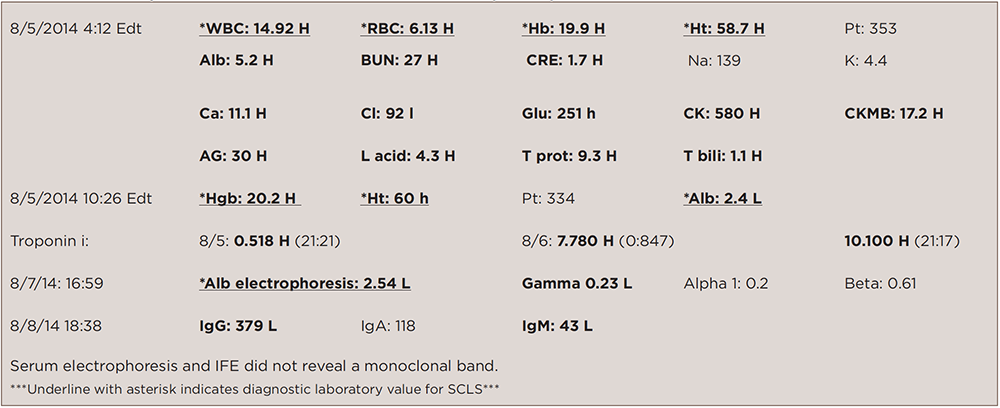
(click for larger image)
TABLE 1: Laboratory Data on Admission & Other Notable Subsequent Inpatient Labs
The patient received 4 liters of intravenous fluids, and within a short amount of time his blood pressure dropped to 69/51. He was immediately transferred to the intensive care unit (ICU). There was concern for sepsis due to ischemic bowel.
In the ICU, he was started on broad-spectrum antibiotics, intubated, given more intravenous fluids with little response, then started on vasopressors. He was taken to the operating room for an explorative laparotomy, which revealed no evidence of perforation.

