Systemic capillary leak syndrome (SCLS) is a very rare disorder, characterized by recurrent episodes of severe hypotension, hypoalbuminemia and hemoconcentration.1 Attacks of SCLS occur in three phases: 1) prodrome; 2) hypovolemia with weight gain; and 3) hypervolemia with fluid overload and polyuria often complicated by pulmonary edema. Often, compartment syndrome can lead to rhabdomyolysis as a serious complication of SCLS.2
As of 2010, 126 cases of SCLS had been reported worldwide, and few cases have been reported since that time.3 No previous literature describes a case of SCLS in a patient with prior rheumatoid arthritis (RA).
Case Presentation
A 58-year-old man with past medical history of RA, gastrointestinal (GI) upset and asthma presented at the emergency department of George Washington Hospital at midnight one summer night in 2014 with severe nausea, vomiting and diffuse abdominal pain and bloating. He denied fever and diarrhea. He reported that he had experienced gastrointestinal upset for two or three days prior to his admission, but his full admitting symptoms had been present only since 6 p.m. the day before.
In 2009, the patient was diagnosed with RA (positive RF and negative cyclic citrullinated peptide). He first presented with hand pain. He was initially treated with methotrexate, but it was discontinued in July 2011 due to GI upset. The patient was then treated with leflunomide, which he was still using daily at time of admission.
In the emergency department, he was noted to have stable blood pressure of 112/74 and a pulse rate of 130. He received intravenous fluids, pain medications and anti-emetics. He had a CT scan of the abdomen notable for a possible early/partial small bowel obstruction.
While in the emergency department, his labs were notable for a white blood cell count of 14.92, hemoglobin 19.9, hematocrit 58.7 and platelet 353. His creatinine was 1.7, albumin 5.2, bicarbonate 17.2, anion gap 30 and lactate 4.3. (See Table 1)
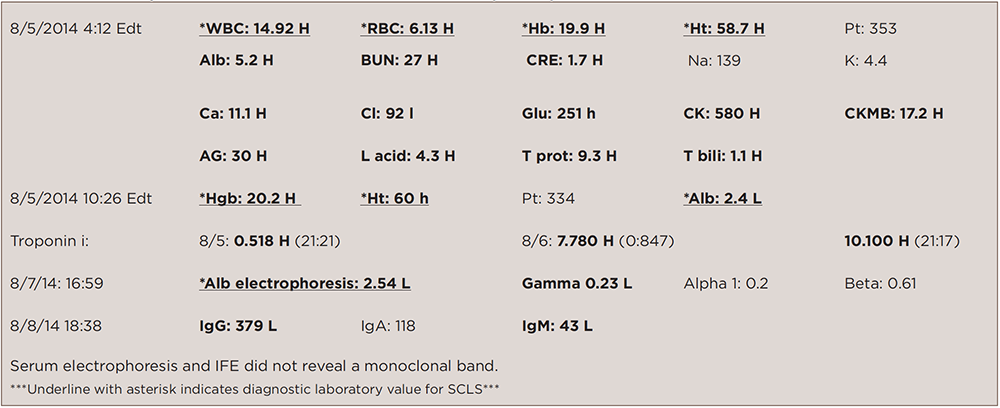
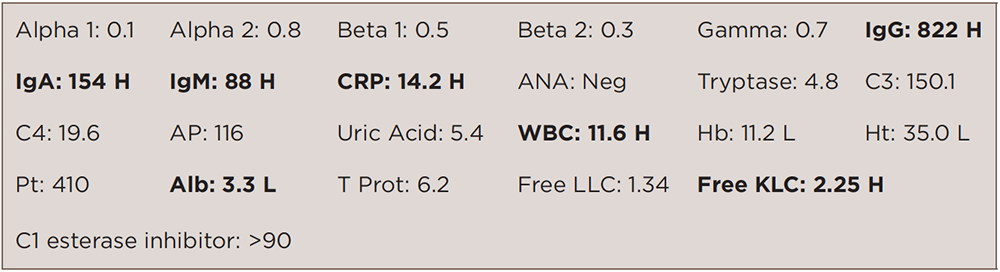
(click for larger image)
TABLE 1: Laboratory Data on Admission & Other Notable Subsequent Inpatient Labs
The patient received 4 liters of intravenous fluids, and within a short amount of time his blood pressure dropped to 69/51. He was immediately transferred to the intensive care unit (ICU). There was concern for sepsis due to ischemic bowel.
In the ICU, he was started on broad-spectrum antibiotics, intubated, given more intravenous fluids with little response, then started on vasopressors. He was taken to the operating room for an explorative laparotomy, which revealed no evidence of perforation.
Repeat labs were notable for white blood cell count of 8.84, hemoglobin 20.2, hematocrit 60, platelets 331. His creatinine was 2.1, albumin 2.4, bicarbonate 13.9, anion gap 26 and lactate 6.1. In the ICU, he was treated supportively, required two vasopressors and stress dose corticosteroids, and received 10 liters of crystalloid fluids, in addition to albumin boluses.
The patient had evidence of abdominal compartment syndrome, requiring an open abdomen after his laparotomy for several days before eventual closure. Also, he suffered from a small cardiac event with a troponin leak to 10.1. An echocardiogram was unremarkable (EF 51%).
Other labs were notable for low IgG (379), IgM (43) and normal IgA (118). Serum electrophoresis was notable for low total protein, hypoalbuminemia (2.54), hypogammaglobulinemia (0.23) and no monoclonal band.
Within the next three days, the patient improved, his abdomen was closed, vasopressors were weaned, and he was extubated. The patient was discharged seven days after admission.
A month later, the patient was taken to the NIH and diagnosed with systemic capillary leak syndrome. In September 2014, he was placed on intravenous immunoglobulin indefinitely. (See Table 2)
The patient’s RA had stayed in remission since October 2013. He was taken off of leflunomide during his hospital course and placed on hydroxychloroquine from September 2014 to January 2015 for his RA. Hydroxychloroquine was discontinued in December 2014, because the patient developed a diffuse rash.
The patient was placed on adalimumab in September 2015 for flare of RA with manifestations of increased hand and foot pain, morning stiffness, four tender joints on 28-joint-count exam plus tender metatarsophalangeal joints.
As of February 2016, the patient’s RA and SCLS remained in remission, and the patient reported maintaining a very active lifestyle.
Discussion
We present a rare case of adult SCLS in a rheumatoid arthritis patient. The diagnosis of SCLS is clinical and may be difficult to recognize and diagnose on initial presentation. Hypotension, hemoconcentration, hypoalbuminemia and the absence of secondary causes of shock are typical. The singular combination of hypotension and elevated hematocrit reflects the profoundly reduced intravascular volume and endothelial barrier dysfunction unique to SCLS.4 The diagnostic evaluation should be performed concurrently with initial fluid management. Immediate intervention should be started because SCLS has a high fatality rate.5 Mortality ranges from 30% to 76%.6,7
The pathogenesis and pathophysiology of SCLS are relatively unknown. Reports suggest that VEGF and angiopoietin 2 (Ang2) contribute to endothelial contraction and may be associated with pathogenesis.8 Further investigations of various biomarkers, which may play an important role, are needed to clarify the pathophysiology of SCLS.5
Monoclonal gammopathies of undetermined significance (MGUS) can support the diagnosis of SCLS, but are not uniformly present.9 Notably, an estimated 79–82% of patients with SCLS have MGUS.3 A monoclonal IgG kappa in a serum sample from this patient was detected on Sept. 11, 2014, together with an elevated kappa/lambda serum-free light chain ratio and beta-2 micro globulin, which support the diagnosis of MGUS. A bone marrow biopsy could be considered for confirmation purposes.
For prophylaxis of recurrent SCLS attacks, many patients, including ours, have received IVIG to successfully remain in remission. Gouseff and Amoura reported anecdotal success with monthly IVIG infusions as prophylactic therapy in three patients.10 Additionally, an NIH study reported that monthly prophylaxis with high-dose intravenous immunoglobulin was associated with a sharp reduction in the number of acute systemic capillary leak syndrome attacks with few side effects in 18 patients. This is an improvement from previously tried theophylline-based therapy, which was frequently associated with breakthrough symptoms and substantial side effects.11 A Swiss Internal Medicine department also reported a case of a 40-year-old woman with chronic SCLS successfully treated with high-dose intravenous immunoglobulins, after a prophylactic therapy with theophylline and terbutaline was poorly tolerated and failed to decrease the frequency and severity of the attacks sufficiently.12
The mechanism of action of IVIG in SCLS is poorly understood.11 Several reports demonstrate evidence of an immune-mediated pathogenesis of SCLS, with increased levels of cytokines, including IL-6, IL-10, interferon-γ and tumor necrosis factor-α.13 IVIG possess anticytokine properties and inhibit the synthesis of different ILs, including IL-2, and may operate in SCLS through modulation of the immune response.14
Lastly, no previous literature describes a case of SCLS in a patient with prior RA. Reports on adult SCLS are few, and accumulation of similar case reports is needed. Particularly, more cases are needed in regard to the relationship of systemic capillary leak syndrome and rheumatoid arthritis and other rheumatic diseases.
 Alexis Smith, MD, is a graduate of Georgetown School of Medicine, Washington, D.C., and a resident in family medicine at Harbor-UCLA Medical Center, Los Angeles, Calif.
Alexis Smith, MD, is a graduate of Georgetown School of Medicine, Washington, D.C., and a resident in family medicine at Harbor-UCLA Medical Center, Los Angeles, Calif.
 Angus Worthing, MD, FACP, FACR, is a practicing rheumatologist in the Washington, D.C., metro area and clinical assistant professor of medicine at Georgetown University.
Angus Worthing, MD, FACP, FACR, is a practicing rheumatologist in the Washington, D.C., metro area and clinical assistant professor of medicine at Georgetown University.
References
- Clarkson B, Thompson D, Horwith M, et al. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960 Aug;29:193–216.
- Milner CS, Wagstaff MJ, Rose GK. Compartment syndrome of multiple limbs: An unusual presentation. J Plast Reconstr Aesthet Surg. 2006;59(11):1251–1252.
- Druey K. Greipp PR. Narrative review: The systemic capillary leak syndrome. Ann Intern Med. 2010 Jul 20;153(2):90–98.
- Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med. 1999 Jun 1;130:905–909.
- Iwasa T, Ohashi H, Kihira K, et al. 10-year-old girl with life-threatening idiopathic systemic capillary leak syndrome: A case report. BMC Pediatr. 2014 May 31;14:137.
- Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med. 1999 Jun 1;130(11):905–909.
- Dhir V, Arya V, Malav IC, et al. Idiopathic systemic capillary leak syndrome (SCLS): Case report and systematic review of cases reported in the last 16 years. Intern Med. 2007;46(12):899–904.
- Xie Z, Ghosh CC, Patel R, et al. Vascular endothelial hyperpermeability induces the clinical symptoms of Clarkson disease (the systemic capillary leak syndrome). Blood. 2012 May 3;119(18):4321–4332.
- Kawabe S, Saeki T, Yamasaki H, et al. Systemic capillary leak syndrome. Intern Med. 2002 Mar;41(3):211–215.
- Gouseff M, Amoura Z. Idiopathic capillary leak syndrome. Rev Med Interne. 2009 Sep;30(9):754–768.
- Xie Z, Chan EC, Long LM, et al. High-dose intravenous immunoglobulin therapy for systemic capillary leak syndrome (Clarkson disease). Am J Med. 2015 Jan;128(1):91–95.
- Zipponi M, Eugster R, Birrenbach T: High-dose intravenous immunoglobulins: A promising therapeutic approach for idiopathic systemic capillary leak syndrome. BMJ Case Rep. 2011 May 3;2011. pii: bcr1220103599.
- Dowden AM, Rullo OJ, Aziz N, et al. Idiopathic systemic capillary leak syndrome: Novel therapy for acute attacks. J Allergy Clin Immunol. 2009 Nov;124(5):1111–1113.
- Andersson UG, Björk L, Skansén-Saphir U, et al. Down-regulation of cytokine production and interleukin-2 receptor expression by pooled human IgG. Immunology. 1993 Jun;79(2):211–216.