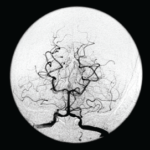
Figure 1: A head CT revealed a subacute infarct involving the right-posterior medial, parietal and occipital lobes.
Case report: A 60-year-old Hispanic male with poorly controlled hypertension was sent from the primary care clinic for evaluation of malignant hypertension with a systolic blood pressure above 200 mmHg. His symptoms at the time of presentation included episodic confusion, worsening vision and an unsteady gait.
A head computed tomography (CT) scan showed a subacute infarct involving the right posterior medial, parietal and occipital lobes (see Figure 1).
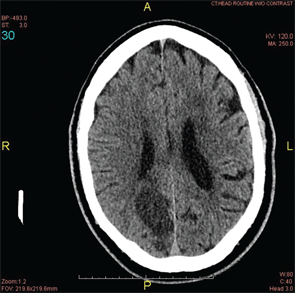
A magnetic resonance imaging (MRI) and magnetic resonance angiogram (MRA) scan were performed. They demonstrated bilateral middle cerebral artery (MCA) stenosis with good collateral circulation and confirmed a subacute right occipito-parietal infarct, involving the splenium (see Figures 2A & 2B).
A CT cerebral angiogram was performed and showed near occlusion of the distal right middle cerebral artery, occlusion of the proximal left MCA and occlusion of the right posterior cerebral artery (see Figure 3).
The patient was started on aspirin, clopidogrel and atorvastatin. After a 14-day hospital course, the patient was discharged to home.
Two weeks later, the patient presented to the emergency department with a new-onset, right-sided facial droop and slurred speech. An MRI at this visit showed an acute lacunar infarct of the left corona radiata (see Figure 4). Despite normal erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), anti-neutrophil cytoplasmic antibody (ANCA) and antinuclear antibody (ANA) tests, there was a concern for CNS vasculitis, and the patient was empirically started on high-dose steroids.
Further workup included the following studies: immunoglobulin levels, complement levels, and cerebrospinal fluid (CSF) analysis for antibodies. All studies were negative. A repeat CT cerebral angiogram revealed long-segment stenosis of both MCAs (see Figures 5A & 5B). At this time, a diagnosis of moyamoya disease was made. The patient was started on warfarin (Coumadin) and discharged to home.
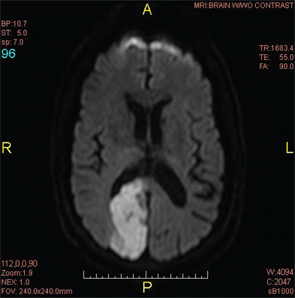
Figure 2A: An MRI of the brain confirmed a subacute infarct involving the right occipito-parietal lobe.
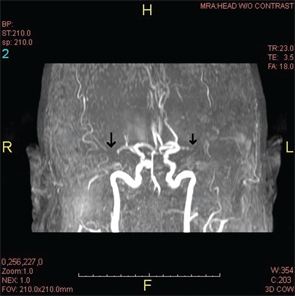
Figure 2B: An MRA revealed the lack of flow in the middle cerebral artery that could be attributed to an occlusion or stenosis.
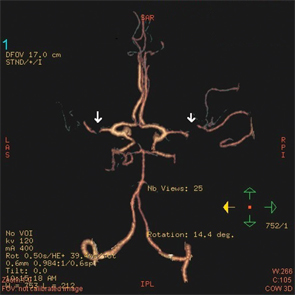
Figure 3: A CT angiogram of the head revealed bilateral MCA stenoses and occlusion of the right posterior cerebral artery.
Discussion
Primary CNS vasculitis, also known as primary angiitis of the CNS (PACNS), and moyamoya disease are both rare causes of stroke and are often indistinguishable in clinical presentation. Although both may present similarly, physicians must learn to differentiate between them, because management for each differs greatly.
For moyamoya disease, no evidence suggests any benefit from corticosteroid therapy.
PACNS is a rare vasculitis that is limited to the brain and the spinal cord. It leads to diverse and non-specific neurological manifestations, with an increase in morbidity and mortality.1