Drug News
A recent phase III, placebo-controlled study of adalimumab in patients (n=185) with active nonradiographic axial spondylarthritis (NRAS) was associated with significant improvements in physical function and health-associated quality of life.1 Patients received adalimumab or placebo for 12 weeks, after which 179 patients continued to receive adalimumab in an open-label manner for 144 additional weeks. After 52 weeks, 77% percent of patients met the minimum important difference for improvement in health-associated quality of life, and around 62% of patients met the minimum important difference for improvement in self-reported physical function. In July 2012, the European Commission approved adalimumab for the treatment of severe NRAS.
New ACR gout guidelines were recently released, stating that xanthine oxidase inhibitors—either allopurinol or the newer febuxostat—can be used first line as urate-lowering therapies. In addition, target serum urate levels should be below 6 mg/dL.2 Allopurinol should still be the first choice for most patients, and it costs only about $15 a month. Since febuxostat is relatively new and “brand only,” it carries a price tag of around $180 a month.3 In clinical trials, only the 80-mg dose of febuxostat was more effective than 600 mg of allopurinol. Hypersensitivity reactions are more common with allopurinol so far, so if patients develop any allergic types of reactions such as itching or a rash, they should discontinue it immediately. Also remember to adjust doses for patients with impaired renal function.
Denosumab has been U.S. Food and Drug Administration (FDA) approved to increase bone mass in men with osteoporosis who are at high risk for fracture.4 There are approximately two million U.S. men who have osteoporosis, with an additional 12 million who are at risk for developing osteoporosis. Osteoporotic fractures and osteoporosis in men remain underdiagnosed and undertreated.
Low-dose, delayed-release prednisone, branded as Rayos in the United States and Lodotra in Europe, was approved earlier this year.5 It is a proprietary formulation of low-dose prednisone. Although the pharmacokinetics of this new formulation differ in its approximate four-hour lag time compared to that of traditional, immediate-release prednisone products, its absorption, distribution, and elimination processes are comparable to immediate-release prednisone. When taken, it should be given with food to improve absorption. Tablets should not be divided, broken, or chewed. Although yet to be seen in clinical practice, it is recommended for 10 p.m. dosing to coincide with middle-of-the-night and early-morning inflammation, when cytokine levels start to rise. Generic prednisone is still a better bet for patients, and the cost is substantially different as well. Rayos costs around $200 a month for 30 tablets of the 5 mg strength, whereas generic prednisone may be as low as $4 at some large discount pharmacies or through $4 generic programs.6
In an abstract of pooled studies presented at the recent 2012 ACR/ARHP Annual Meeting in Washington D.C., tofacitinib, the new oral janus kinase inhibitor, appeared to have efficacy in the treatment of rheumatoid arthritis (RA) patients with disease refractory to tumor necrosis factor–alpha (TNF) inhibitors.7 ACR20 responses for patients who failed one TNF inhibitor occurred in 44% and 50% of patients, respectively, receiving 5 mg tofacitinib twice daily (BID) and 10 mg BID, versus 24% of placebo-treated patients (P<0.0001). For patients who failed two TNF inhibitors, 41% of tofacitinib 5-mg BID-treated patients and 53% tofacitinib 10-mg BID-treated patients were ACR20 responders, versus 16% of placebo patients (P<0.01 for 5 mg; P<0.0001 for 10 mg).
Drug Safety
Methotrexate/Proton Pump Inhibitors
On October 30, 2012, the FDA approved supplemental information on the pharmacokinetics of using milnacipran (Savella) in lactating women.8 The data reported that milnacipran is present in the milk of lactating women treated with the agent. Lactating women (n=8) who were at least 12 weeks postpartum and were weaning their infants received a single, oral dose of 50 mg milnacipran. The maximum estimated daily infant dose for milnacipran from breast milk was 5% of the maternal dose based on peak plasma concentrations. In most patients, peak concentrations of milnacipran in breast milk were seen within four hours after the maternal dose. Based on this data, the product information was updated to recommend that due to the limited amount of data regarding infant exposure to milnacipran, it should be used cautiously in nursing women.
In October 2012, the FDA updated the Warnings and Precautions section of the label for tocilizumab (Actemra) related to hypersensitivity reactions, including anaphylaxis.9 Postmarketing, clinically significant hypersensitivity, and anaphylaxis reactions have occurred both with and without previous hypersensitivity reactions in patients treated with the agent. Reactions have occurred in patients receiving a range of doses, and in some cases, this has occurred with the first tocilizumab infusion. Some of these reactions have led to fatalities, and events even have occurred in patients who were premedicated. If anaphylaxis or other clinically significant hypersensitivity reaction occurs, administration of tocilizumab should be stopped immediately, and tocilizumab should be permanently discontinued.10
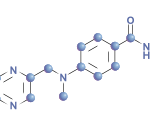
There is accumulating evidence suggesting that combined use of methotrexate (MTX; at both low and high doses) and proton pump inhibitors (PPIs) may reduce the clearance of MTX, leading to elevated and prolonged serum MTX levels, and/or levels of its metabolite hydroxymethotrexate, possibly leading to methotrexate toxicities.11 Implicated PPIs include omeprazole, esomeprazole, and pantoprazole, but other PPIs may also cause this same interaction (e.g., a class effect) because this interaction has been described for different PPIs. PPIs are often used in patients with RA to reduce nonsteroidal antiinflammatory–associated gastric ulcers, to treat gastric ulcers and manage gastroesophageal reflux disease, as well as to manage gastrointestinal side effects of MTX.
Through a study of the Adverse Events Reporting system (AERS) and a literature review, Bezabeh et al identified reports of this potential interaction.11 Most patients were receiving high-dose MTX for cancer indications, but other indications included psoriatic arthropathy, pulmonary fibrosis, and RA, where lower MTX doses were used. When the AERS reports were evaluated, reactions included renal toxicity, hematologic events, and myopathy, and two of those case reports suggested that the PPI interfered with the elimination of MTX. Since PPIs are used extensively, healthcare practitioners need to be aware of this potential interaction. In several of the case reports evaluated, elimination of MTX normalized when the drug was removed. Additionally, when an H-2 receptor blocker was substituted for the PPI, no MTX toxicity was identified. When an H-2 receptor blocker was then stopped and the PPI was restarted, the MTX toxicity reappeared (a positive rechallenge). Although no formal studies have been conducted on this potential interaction and subsequent MTX toxicity, evidence of disappearance of the reaction upon drug discontinuation and/or reappearance of the reaction upon rechallenge are strong suggestions of causality. This possible drug–drug interaction has been added to the labels for intravenous MTX and for PPIs.
In patients where gastric acid suppression is clinically indicated during MTX therapy, clinicians should consider substituting an H-2 receptor blocker (e.g., famotidine, ranitidine, nizatidine) for a PPI. The H-2 receptor blocker cimetidine might not be a good choice due to its numerous potential drug interactions. Clinicians are also encouraged to report any suspected cases of this potential drug–drug interaction, leading to MTX toxicity or other potential drug-induced events, to the FDA MedWatch program at www.fda.gov/medwatch.
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City, a clinical pharmacist at New York Downtown Hospital, and adjunct faculty at Touro College of Pharmacy.
References
- Barber J. Abbott presents positive phase III results for Humira in axialspondyloarthritis. Published November 12, 2012. Available at www.firstwordpharma.com/forward/emailref?path=node/1032194. Accessed November 13, 2012.
- Walsh N, Jasmer R, Caputo D. ACR Puts Out Gout Guidelines. Published September 29, 2012. Available at www.medpagetoday.com/Rheumatology/GeneralRheumatol ogy/35033. Accessed November 28, 2012.
- Febuxostat (Uloric) for Chronic Treatment of Gout. The Medical Letter on Drugs and Therapeutics. May 18, 2009;51:37-38.
- FDA Approves New Indication for Prolia (Denosumab) for the Treatment of Bone Loss in Men with Osteoporosis at High Risk for Fracture. Published September 20, 2012. Available at www.ext.amgen.com/media/media_pr_detail.jsp?year=2012&releaseID=1737204. Accessed November 28, 2012.
- Horizon Pharmaceuticals. Horizon Pharma announces FDA approval of Rayos (prednisone) delayed-release tablets for rheumatoid arthritis and multiple additional indications. Published July 26, 2012. Available at http://ir.horizon-pharma.com/releasedetail.cfm?ReleaseID=695983. Accessed December 7, 2012.
- Rayos. The Medical Letter on Drugs and Therapeutics. November 26, 2012;54:94.
- Walsh N, Agus ZS. Tofacitinib succeeds in refractory disease. Published November 15, 2012. Available at www.medpagetoday.com/MeetingCoverage/ACR/35964. Accessed November 16, 2012.
- Savella (milnacipran HCl) tablets. Published October 2012. Available at www.fda.gov/Safety/MedWatch/Safety Information/ucm203615.htm. Accessed December 6, 2012.
- Actemra (tocilizumab) injection for intravenous infusion. Published October 2012. Available at www.fda.gov/Safety/MedWatch/SafetyInformation/ucm327824.htm. Accessed November 29, 2012.
- Actemra label. Published November 11, 2012. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2012/125276s0049lbl.pdf. Accessed November 29, 2012.
- Bezabeh S, Mackey A, Kluetz P, Jappar D, Korvick J. Accumulating evidence for a drug-drug interaction between methotrexate and proton pump inhibitors. Oncologist. 2012;17:550-554.