ajt/shutterstock.com
Medications for serious or life-threatening conditions may receive accelerated approval from the U.S. Food and Drug Administration (FDA) by showing an effect on surrogate measures that are reasonably likely to predict a treatment’s clinical benefit. Post-approval confirmatory drug trials are then required to determine whether or not these effects translate into clinical improvements. In recent years, the number of drugs that have received FDA accelerated approval has increased.
When drugs undergo the accelerated approval process, the concern is that the safety and efficacy of these agents are not well established. Additional concern exists because this safety and efficacy information may not be confirmed during three-year, post-drug-approval trials. Some clinicians believe the drugs undergoing the accelerated approval process may pose a greater risk to patients, while others look toward proven effectiveness, rather than just surrogate markers of efficacy.
In a recent study, researchers evaluated the characteristics of drugs that received FDA accelerated approval between 2009 and 2013.1 They reviewed publicly available FDA documents used in the preapproval trials that led to the accelerated drug approvals to determine the characteristics of the drugs receiving this approval. The FDA’s post-marketing database of requirements, commitments and matched, peer-reviewed publications was also used to obtain needed information. The study follow-up ended on April 7, 2017. Its design features a comparison of the preapproval and confirmatory studies. Subsequent regulatory decisions and estimated time between accelerated approval and fulfillment of regulatory requirements were also summarized.
The Results: During the evaluated timeframe, the FDA granted accelerated approval to 22 drugs for 24 indications, with 38 preapproval studies supporting 24 indications. Nineteen indications were for oncologic treatment. Of the required post-approval confirmatory studies, 19 of 38 (50%) were completed in a minimum of three years post-approval. Of these studies, most showed some treatment benefit, but relied on surrogate measures rather than clinical outcomes. Twenty-five of the 38 (66%) studies observed clinical efficacy, seven (18%) evaluated longer follow-up and six (16%) evaluated safety. The proportion of randomized studies did not differ before and after accelerated approval.
Efficacy was demonstrated for 10 of 24 (42%) indications in completed studies that used surrogate measures. As a result, the package inserts (e.g., drug labels) of these medications were updated. Of the 14 of 24 (58%) indications that had not completed all the requirements, at least one of the confirmatory studies did not demonstrate a clinical benefit, two (8%) were terminated and three (13%) were delayed by more than one year.
For the remaining seven indications (29%), studies were progressing according to target timelines. Clinical benefit had not yet been confirmed for eight indications that had been initially approved at least five years prior. The most common surrogate measure in the preapproval studies was disease response, because many drugs were cancer agents. Other surrogate measures included time-to-event outcomes, such as progression-free survival and time-to-sputum culture conversion; and change in baseline biomarker levels, such as liver iron concentration. Most requirements were for randomized clinical trials (n=25); the rest (n=13) were single-group studies, including long-term extensions of preapproval studies.
Among the 22 drugs with 24 indications granted FDA accelerated approval in the studied timeframe, efficacy was often confirmed in post-approval trials a minimum of three years after approval in most studies. The confirmatory and preapproval trials had similar study elements, including using surrogate measures as outcomes. Although this type of evaluation has many limitations, the information can be useful in evaluating post-marketing safety and effectiveness for use in patients.
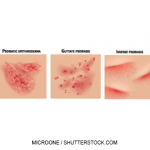
Secukinumab Meets 5-Year Benchmark for Psoriasis
In 2015, the FDA approved secukinumab (Cosentyx), the first fully human IL-17A inhibitor approved to treat psoriasis, psoriatic arthritis (PsA) and ankylosing spondylitis (AS).2 And data recently presented at the 26th European Academy of Dermatology and Venereology (EADV) Congress in Geneva, Switzerland, demonstrates sustained efficacy and safety. The research in patients with moderate to severe plaque psoriasis showed that secukinumab conveyed a high rate of and long-lasting skin clearance at five years.
In the SCULPTURE study, Psoriasis Area and Severity Index (PASI) 75 responders at Week 12 were randomized to double-blind maintenance treatment of 300 or 150 mg secukinumab given at a four-week, fixed-interval regimen or as needed. Patients who completed 52 weeks of the SCULPTURE study (N=642) were eligible to continue the same dose and regimen in the extension study. The five-year extension study (A2304E1) is a multicenter, double-blind and open-label extension of the Phase 3 SCULPTURE study.
The primary objective of the open-label extension was to assess the long-term safety and tolerability of secukinumab in patients with moderate to severe plaque psoriasis. Efficacy measures were the proportion of patients achieving PASI 75, PASI 90 and PASI 100. At Year 1, the PASI 75 response rate was 89%, and the PASI 90 response rate was 69%. This high rate was maintained at Year 5, with a PASI 75 response rate of 89% and a PASI 90 response rate of 66%. Additionally at Year 1, 44% of psoriasis patients achieved completely clear skin (PASI 100), and this rate was maintained to Year 5 (41%). The drug continued to exhibit a favorable and consistent safety profile, with low immunogenicity.
Michele B. Kaufman, PharmD, BCGP, is a freelance medical writer based in New York City and a pharmacist at New York Presbyterian Lower Manhattan Hospital.
References
- Naci H, Smalley K, Kesselheim A. Characteristics of preapproval and postapproval studies for drugs granted accelerated approval by the U.S. Food and Drug Administration. JAMA. 2017 Aug 15;318(7):626–636.
- Novartis. Press release: Novartis’ Cosentyx sets new benchmark in psoriasis with robust five-year sustained Phase III efficacy and safety data. 2017 Sep 19.