
gwolters / Shutterstock.com
Case
Ms. A is an 82-year-old woman who presented to the rheumatology office for evaluation of osteoporosis. She had been diagnosed with postmenopausal osteoporosis at age 62 after sustaining a right wrist fracture. She was started on alendronate 70 mg weekly and reported medication compliance. At age 79, she sustained an atraumatic right femur fracture. She was continued on alendronate at the same dosage by Physician 1. Three years later, she sustained a third fracture, an atraumatic left femur fracture.
An orthopedic surgeon repaired the left femoral fracture and referred her to a rheumatologist, Physician 2, for the management of her osteoporosis. The patient had no other medical problems. Physician 2 reviewed X-rays taken at the time of each of her femoral fractures. Each femoral fracture had a similar radiographic appearance, consistent with an atypical femoral fracture (AFF) (see Figure 1). Physician 2 discussed the diagnosis of AFFs with the patient and recommended discontinuation of alendronate, which she had taken for the past 20 years. Physician 2 recommended that she initiate a two-year course of teriparatide 20 mcg daily. The patient expressed concern about the decision of her former physician (Physician 1) to continue alendronate despite the fact that she had sustained a right femoral fracture at age 79. She was concerned that her medication continuation might have contributed to her developing a second AFF, on the contralateral side.
What should Physician 2 do next?
Discussion
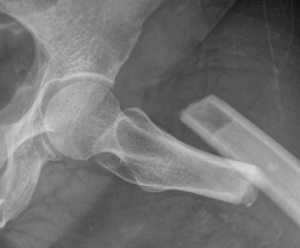
Figure 1: Subtrochanteric transverse fracture consistent with a left atypical femoral fracture.
Medical errors are defined as the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim.1 Adverse events are injuries that result from a medical intervention and are responsible for harm to the patient.1 When medical errors lead to adverse events in patients, physicians should disclose them to their patients. A full disclosure of medical error involves communication between the healthcare provider and patient that includes admission of a mistake, discussion of the error and a conversation about the link from error to harm.2
Medical societies in the U.S. support full disclosure of medical errors that lead to adverse events.3,4 For example, the American Medical Association code of ethics states: “Situations occasionally occur in which a patient experiences significant medical complications that may have resulted from the physician’s mistake or judgment. Therefore, the physician is ethically required to inform the patient of all the facts necessary to ensure understanding of what has occurred.”4
Several reasons exist for the disclosure of medical errors that lead to adverse events. First, physicians have an ethical duty to be honest. Second, the disclosure of medical errors is essential for informed consent in future patient care medical decisions. Hence, the disclosure of medical errors will enhance patient trust in physicians. Last, the disclosure of medical errors is important in physician to physician education, which helps prevent future similar events.
Although there is general agreement that physicians should disclose their errors, literature regarding disclosure of another physician’s error(s) remains scarce. Although there is support in the literature to disclose medical errors made by other physicians, several unique barriers regarding disclosure of another physician’s error exist.5,6
One obstacle relates to limited information. The current physician may not have been directly involved in the care of the patient when the error occurred. An error may have contributed to an adverse event, but may not have been the sole cause of the adverse event. Therefore, it may be difficult to establish causal inference in the setting of limited information. Second, given different practice patterns, there may not be agreement on what constitutes an error. Certain practice patterns may be well within the scope of acceptable practice although not representative of personal decision making. Third, there is fear of exposing one’s colleague to malpractice litigation with disclosure of a medical error. Therefore, for many reasons, physicians may avoid disclosing a colleague’s error.
Good communication between physicians is critical in overcoming barriers to limited information and disagreement around what constitutes an error. Physician 2 could initiate dialogue with Physician 1 to distinguish the rationale for continuing alendronate for the duration of Ms. A’s therapy, as well as its continuation following the first AFF. Physician 2 could begin the conversation in a curious and exploratory manner with the goal of determining Physician 1’s medical decision making. The next steps would then depend largely on this discussion’s course and outcome. Physician 1’s decision to treat with prolonged bisphosphonates may have been related to the patient’s fracture risk. Physician 1 may not have recognized the first fracture as an AFF.
Therefore, the first step for Physician 2 is to investigate the course of events further, and this best ensues through direct communication between physicians. Direct communication between physicians also provides an opportunity for physician-to-physician education, mitigating against future similar medical errors.
In the unfortunate situation of determining that an error has occurred, one should disclose the error, even if it involves another physician. The patient has the right to know that prolonged alendronate treatment may have been associated with her first AFF and continuation of the medication may have contributed to the second AFF. Who should be responsible for the disclosure? Gallagher and colleagues suggest that this disclosure decision should take into account many factors including who has the strongest relationship with the patient, who has the best understanding of what happened and its implication for the patient, who is responsible for patient care, and who has the most experience with the disclosure in complex situations.7 If both physicians practice in the same institution, then joint disclosure would be ideal.
In the case of physicians from different institutions, close coordination of the disclosure process is warranted. Physician 2 has an ethical obligation to disclose that long-term alendronate use has been associated with the occurrence of AFFs and may similarly have contributed to the second AFF. After obtaining information about Physician 1’s medical decision making and coordinating communication between medical directors from both institutions, Physician 2 and the institution’s medical director should disclose that alendronate may have contributed to both AFFs.7 Physician 1 should be provided the opportunity to be involved in the disclosure process.
Adequate preparation for the effective disclosure of medical errors is important. Many physicians may lack sufficient training to handle complex and challenging disclosure conversations. Before patient disclosure, the medical team should reach a consensus around the events and decisions that have occurred. The physician should objectively disclose the facts to the patient, subordinating their emotions and ego, in a timely and expedited fashion to maintain trust in the patient–physician relationship. Physicians should seek emotional support via professional counseling and from colleagues after disclosing a medical error, recognizing that error disclosures may lead to significant physician emotional distress.8
As we strive toward building a safer medical system, providing a legal framework that promotes honest disclosure of errors is critical. The Patient Safety and Quality Improvement Act of 2005 provides confidentiality protection for discussion of medical errors within a system of patient safety organizations and a national patient safety database. Nevertheless, many shortcomings remain in the laws that protect healthcare providers who disclose medical errors from litigation.9 Many states have enacted disclosure laws to provide legal protection to physicians who disclose medical errors. However, many states provide protection only to the expression of sympathy after an error, but are not protective of statements of acceptance of responsibility. Notably, there is significant variability between state disclosure laws.
Institutions play a fundamental role in promoting a positive atmosphere for honest disclosure of errors to improve patient safety. Although litigation fear remains a critical barrier for physicians disclosing medical errors, recent studies show that increased disclosure of medical errors, within the context of a disclosure program, does not result in increased legal claims and costs.10,11 For example, implementation of a disclosure-with-offer program at the University of Michigan (compensation offered to patients when an internal investigation reveals medical error) did not increase legal claims and costs.10 Institutions should see errors as an opportunity for system improvement to provide safer care, a critical component of quality improvement programs and a mechanism to improve patient outcomes. Institutions should also strive to provide a disclosure support framework, including basic disclosure training and disclosure coaches who provide technical and emotional support to physicians regarding the disclosure process.11 Promoting conversations between clinicians and providing avenues (both formal and informal) for addressing and discussing errors are vital in supporting a positive disclosure environment.
In summary, despite the multiple challenges of disclosing another physician’s error, disclosure remains the right thing to do. Efforts should be made to ensure a meaningful disclosure process for the physician, patient and institution as we continue to reinforce a safe, patient-centered healthcare system built on honesty and trust among its participants.
 Sian Yik Lim, MD, is a rheumatologist at the Straub Bone & Joint Center, Straub Medical Center, Honolulu. He is a clinical densitometrist certified by the International Society for Clinical Densitometry. He is interested in quality improvement in healthcare and has been involved in efforts to improve the quality of osteoporosis care in Hawaii. Follow him on Twitter: @limsianyik.
Sian Yik Lim, MD, is a rheumatologist at the Straub Bone & Joint Center, Straub Medical Center, Honolulu. He is a clinical densitometrist certified by the International Society for Clinical Densitometry. He is interested in quality improvement in healthcare and has been involved in efforts to improve the quality of osteoporosis care in Hawaii. Follow him on Twitter: @limsianyik.
 Marcy B. Bolster, MD, is an associate professor of medicine, Harvard Medical School, Boston. She is the director of the Rheumatology Fellowship Training Program at the Massachusetts General Hospital (MGH) and is the medical lead for the MGH Fracture Liaison Service. She is a clinical densitometrist certified by the International Society for Clinical Densitometry.
Marcy B. Bolster, MD, is an associate professor of medicine, Harvard Medical School, Boston. She is the director of the Rheumatology Fellowship Training Program at the Massachusetts General Hospital (MGH) and is the medical lead for the MGH Fracture Liaison Service. She is a clinical densitometrist certified by the International Society for Clinical Densitometry.
Disclosures: Dr. Lim reports no potential conflicts of interest. Dr. Bolster has received a research grant from Eli Lilly and has stock investments in Johnson & Johnson.
References
- Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: 2000.
- Fein SP, Hilborne LH, Spiritus EM, et al. The many faces of error disclosure: A common set of elements and a definition. J Gen Intern Med. Jun 2007;22(6):755–761.
- Snyder L; American College of Physicians Ethics, Professionalism, and Human Rights Committee. American College of Physicians Ethics Manual: sixth edition. Ann Intern Med. 2012 Jan 3;156(1 Pt 2):73–104.
- Code of Medical Ethics of The American Medical Association: Current Opinions with Annotations 2012–2013. Chicago: American Medical Association, 2012.
- Moffatt-Bruce SD, Denlinger CE, Sade RM. Another surgeon’s error: Must you tell the patient? Ann Thorac Surg. 2014 Aug; 98(2):396–401.
- Rubin MA, Friedman DI. The ethics of disclosing another physician’s medical error. Continuum (Minneap Minn). 2015 Aug; 21(4 Headache):1146–1149.
- Gallagher TH, Mello MM, Levinson W, et al. Talking with patients about other clinicians’ errors. N Engl J Med. 2013 Oct 31; 369(18):1752–1757.
- Christensen JF, Levinson W, Dunn PM. The heart of darkness: The impact of perceived mistakes on physicians. J Gen Intern Med. 1992 Jul–Aug;7(4):424–431.
- Mastroianni AC, Mello MM, Sommer S, et al. The flaws in state ‘apology’ and ‘disclosure’ laws dilute their intended impact on malpractice suits. Health Aff (Millwood). 2010 Sep;29(9):1611–1619.
- Kachalia A, Kaufman SR, Boothman R, et al. Liability claims and costs before and after implementation of a medical error disclosure program. Ann Intern Med. 2010 Aug 17;153(4):213–221.
- Gallagher TH, Studdert D, Levinson W. Disclosing harmful medical errors to patients. N Engl J Med. 2007 Jun 28;356(26):2713–2719.
