AlexLMX / shutterstock.com
In our fast-paced world, a great deal can happen in 12 months. Reflecting on this past year and my service as ACR president, I find this has certainly been the case.
For the foreseeable future, it appears the factors that influence our ability to effectively care for our patients with rheumatic and musculoskeletal disease will have less to do with scientific advances and the development of new therapies than with the policies and economics of healthcare. Thus, the ACR advocacy team has certainly had a busy year; legislative and policy issues have required major and ongoing attention.
Challenging Policy Landscape
I am continually impressed by the nimbleness and effectiveness of the public affairs and media relations staff and the volunteers of the ACR Government Affairs Committee who rapidly deal with complex issues as they arise. Unfortunately, the satisfaction that came earlier this year from achieving success on several legislative initiatives the ACR strongly supported (e.g., repealing the annual caps on physical therapy, repealing IPAB and preventing quality program payment adjustments from being applied to Part B drug reimbursement) was short-lived. In their place, new—and potentially much more pressing—issues have arisen.
The recent precipitous proposal made by the new administrator of the Centers for Medicare & Medicaid Services (CMS) to collapse evaluation and management (E/M) codes, ostensibly to reduce physician documentation burden, clearly devalues the complex care provided by rheumatologists and other cognitive specialties. In addition, the just-announced plan to expand step therapy to Medicare Advantage will make it increasingly difficult for physicians—and likely patients and their families—to ensure a patient will receive the most appropriate treatment. These policies suggest that cost-cutting efforts will be directed at physicians over other important drivers of healthcare cost.
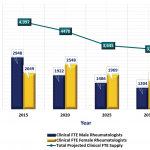
We need to be concerned about policies that undervalue and degrade the practice of rheumatology. Such policies have the potential to negatively impact recruitment to our specialty and exacerbate workforce shortages.
We must also remain alert to efforts to change the Affordable Care Act with policies that reduce patient access to needed care.
These challenges underscore the necessity of ongoing engagement in advocacy by the ACR and by members of our specialty.
In the face of these challenges to healthcare delivery, the ACR continues to lead the way in defining quality care in rheumatic diseases. The Quality of Care Committee (QOC) organizes a wide and expanding range of quality programs, such as development of treatment guidelines. Utilization of comprehensive literature review and a rigorous grading process help ensure ACR treatment guidelines are evidence based and free of external bias. However, given the general paucity of high-grade comparative data, producing timely and clinically meaningful treatment guidelines is a challenge that requires a lot of focused work by many dedicated individuals.