AlexLMX / shutterstock.com
In our fast-paced world, a great deal can happen in 12 months. Reflecting on this past year and my service as ACR president, I find this has certainly been the case.
For the foreseeable future, it appears the factors that influence our ability to effectively care for our patients with rheumatic and musculoskeletal disease will have less to do with scientific advances and the development of new therapies than with the policies and economics of healthcare. Thus, the ACR advocacy team has certainly had a busy year; legislative and policy issues have required major and ongoing attention.
Challenging Policy Landscape
I am continually impressed by the nimbleness and effectiveness of the public affairs and media relations staff and the volunteers of the ACR Government Affairs Committee who rapidly deal with complex issues as they arise. Unfortunately, the satisfaction that came earlier this year from achieving success on several legislative initiatives the ACR strongly supported (e.g., repealing the annual caps on physical therapy, repealing IPAB and preventing quality program payment adjustments from being applied to Part B drug reimbursement) was short-lived. In their place, new—and potentially much more pressing—issues have arisen.
The recent precipitous proposal made by the new administrator of the Centers for Medicare & Medicaid Services (CMS) to collapse evaluation and management (E/M) codes, ostensibly to reduce physician documentation burden, clearly devalues the complex care provided by rheumatologists and other cognitive specialties. In addition, the just-announced plan to expand step therapy to Medicare Advantage will make it increasingly difficult for physicians—and likely patients and their families—to ensure a patient will receive the most appropriate treatment. These policies suggest that cost-cutting efforts will be directed at physicians over other important drivers of healthcare cost.
We need to be concerned about policies that undervalue and degrade the practice of rheumatology. Such policies have the potential to negatively impact recruitment to our specialty and exacerbate workforce shortages.
We must also remain alert to efforts to change the Affordable Care Act with policies that reduce patient access to needed care.
These challenges underscore the necessity of ongoing engagement in advocacy by the ACR and by members of our specialty.
In the face of these challenges to healthcare delivery, the ACR continues to lead the way in defining quality care in rheumatic diseases. The Quality of Care Committee (QOC) organizes a wide and expanding range of quality programs, such as development of treatment guidelines. Utilization of comprehensive literature review and a rigorous grading process help ensure ACR treatment guidelines are evidence based and free of external bias. However, given the general paucity of high-grade comparative data, producing timely and clinically meaningful treatment guidelines is a challenge that requires a lot of focused work by many dedicated individuals.
A recent review of progress on the five-year guideline development plan indicates the program has met its benchmarks, even while taking on new projects. The Quality of Care Committee and the Guidelines Subcommittee have renewed their efforts to produce guidelines that are useful and relevant to practicing rheumatology providers.
Provision of high-value care is an increasingly important aspect of defining quality care. Although we see the value we provide to patients and the healthcare systems in which we work, documenting and quantifying this value is not easy. The Rheumatology Informatics System for Effectiveness (RISE) registry was developed as a certified Quality Care Data Registry to provide rheumatology practices the ability to document their provision of quality care. The fact that 100% of practices that submitted their Merit-Based Incentive Payment System (MIPS) data via RISE qualified as exceptional performers in their first year of reporting indicates that rheumatologists are, in fact, providing high-quality care and that the investment in building the registry has provided significant value to practicing rheumatologists.
RISE has become the largest source of real-world, clinical data on rheumatology care in the world and will be an increasingly important and useful source for understanding and documenting quality and high value care in the rheumatic diseases. The registry is also a highly visible example of the way in which the ACR and its members are driving innovation and progress in healthcare.
From the very beginning, innovation & rheumatology have gone hand in hand.
Rheumatology Past, Present, Future
From the very beginning, innovation and rheumatology have gone hand in hand. Basic research discoveries in immunology attracted clinicians and physician scientists to define an entirely new specialty. Further stimulating the specialty is the ongoing research in rheumatic and musculoskeletal diseases that have led to life-changing therapies and many new insights into etiology, diagnosis and treatment of some of the most intractable diseases.
Innovation is also apparent in the way we learn and teach, and examples of novel and cutting-edge educational methods by rheumatology educators abound. Ongoing inquiry and learning are intrinsic aspects of the practice of rheumatology.
These features of our specialty have not gone unnoticed by our youngest learners. The progress in our field has been accompanied by a surge in interest in rheumatology training. Securing rheumatology fellowship training through the Match has recently become nearly as competitive as the most popular internal medicine specialties, and training programs are seeing a surge of interest, increased numbers of applications and more highly qualified applicants than ever.
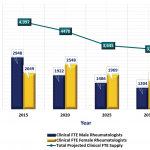
This attention is excellent news for our specialty. The trend also bodes well for our patients and can help serve to maintain and, hopefully, expand the rheumatology workforce. Although current healthcare policy makers don’t appreciate the workforce issue in rheumatology, anyone in practice knows a shortage of rheumatologists already exists. Our projections indicate demand will continue to outpace the availability of trained rheumatologists.
The shortage of physician scientists is likely to become even more acute. This reality emphasizes the importance of working to generate similar interest in the field among allied physician assistants and nurse practitioners, of advocating for more training positions for adult and pediatric rheumatology fellows, and of supporting programs to foster the careers of young physician scientists. It also underscores the importance of advocating against measures that increase the burden and threaten the viability of rheumatology practice.
Impact of Change
Progress can be rapidly halted. We experienced such an effect in the 1990s, when the adoption of the primary care gatekeeper model by managed care and inaccurate workforce projections predicting an excess of rheumatologists led to a drop in rheumatology fellowship applications. Thus, we must continue to advocate for rheumatology training and practice.
The arrival of younger generations of rheumatology providers in the workforce also will affect the field. These talented and idealistic professionals will accelerate innovation and bring new energy to the specialty, and the responsibility lies with us to foster their careers and accommodate their needs and goals. This is a major reason why the ACR has adopted a plan for moving younger members into leadership roles—a plan that is already showing success.
Finally, change will inevitably come as we identify a new executive vice president (EVP) to lead the vision and the talented staff and operations of the ACR. The success and innovation the ACR has achieved over the past 30 years is due, in no small part, to the leadership of Mark Andrejeski, who has served as the EVP over this entire period of time. It is now the responsibility of the search committee and Board of Directors to identify a new executive who can effectively manage and innovate to meet coming challenges.
Of course, challenges spawn opportunity. To realize and optimize our opportunities we must be proactive in identifying and promoting the quality and value we bring to medical research into the rheumatic and musculoskeletal diseases and the and clinical care we provide patients. The precipitous actions by policy makers that we that we are seeing now underscore the need to become more involved as individuals in advocating for our specialty and for our patients. We must continue to work together as a single organization of community-based clinicians, academicians and allied health professionals in support of our common goals and our patients.
David I. Daikh, MD, PhD, is the 81st president of the ACR. Dr. Daikh serves as the director of the Rheumatology Fellowship Training Program at the University of California, San Francisco, and as chief of the Rheumatology Division at the SFVA Medical Center, where he directs the Rheumatology Clinic.