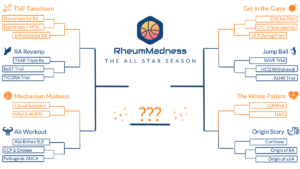
RheumMadness is an online tournament in which a bracket of teams, representing key learning concepts in rheumatology, compete against each other in a series of head-to-head matchups, much like basketball teams in the NCAA’s March Madness.
The 2023 tournament theme was The All Star Season. Each team represented one all star article competing to be named the most important and transformational article ever written in the field of rheumatology. Here, we feature the scouting reports from this year’s Final Four:
- Cortisone, by the University of Colorado Fellowship Program—the winner
- Etanercept for RA, by the Ohio State Fellowship Program
- Autoantibodies Before SLE, by the Massachusetts General Hospital Fellowship Program
- RAVE Trial, by the Wake Forest Fellowship Program
To see all the scouting reports, visit https://sites.duke.edu/rheummadness. RheumMadness is supported by a Clinician Scholar Educator Award from the Rheumatology Research Foundation and modeled after the NephMadness tournament in nephrology.
Rheum on the Rocks
Origins of corticosteroid treatment
BY SMARIKA SAPKOTA, MD, DAVID DEFRANCISCO, MD, & JASON KOLFENBACH, MD
Base Article
Hench PS, Kendall EC, Slocumb CH, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949 Apr 13;24(8):181–197.1
Team Overview
Philip Hench and colleagues published their landmark study in 1949, during an era in which knowledge about the pathologic underpinnings of rheumatoid arthritis (RA) was limited, as were treatment options. Patients at that time were treated with aspirin (first distributed by Bayer in 1899) or, much less commonly, gold or sulfonamide compounds (1930s), often with limited success.2,3 The initial use of sulfonamide compounds, such as sulfasalazine, as well as such medications as d-penicillamine (1950s), reflected a prevailing hypothesis that RA was a microbial-driven disease.
Hench et al. demonstrated remarkable clinical and laboratory improvements in RA disease control through administration of their “Compound E” (17-hydroxy-11-dehydrocorticosterone) to 14 patients with severe RA. This study was critical to the field of rheumatology not only for the discovery of an effective therapeutic agent (i.e., cortisone), but also because it supported a biochemical basis of disease rather than a microbial origin.
Prior to publication of this study, Hench had studied the beneficial effects of pregnancy and jaundice on RA. The improved disease activity he observed in these settings was a novel finding because RA was previously thought to be an irreversible disease. Based on his observations, he sought a common biochemical denominator between pregnancy and jaundice that could lead to a potential therapeutic intervention for RA. After a series of trial-and-error experiments, the team settled on an adrenal hormone as the most likely “anti-rheumatic substance X,” and on Sept. 21, 1948, began treating their first patient with Compound E.