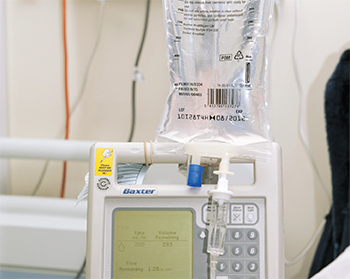
An Intravenous infusion (IV drip) of rituximab is being performed in a hospital setting.
Dr P. Marazzi/Science Source
Rheumatologists prescribe rituximab for induction and maintenance treatment for anti-neutrophil cytoplasm antibody (ANCA) associated vasculitides (AAV). Maintenance treatment typically employs fixed-schedule dosing, but in the recent maintenance of remission using rituximab in systemic ANCA-associated vasculitis II (MAINRITSAN2) trial, researchers from the French Vasculitis Study Group examined whether individually tailored maintenance dosing might work better.
“The main objectives of the MAINRITSAN2 trial were to determine whether an individually tailored infusion strategy would maintain remission with fewer relapses, fewer infusions and fewer infections,” says Loïc Guillevin, professor in the Department of Internal Medicine at Hôpital Cochin at Université Paris Descartes, France. “The other objective was to determine whether a reinfusion strategy based on ANCA and circulating CD19+ B cells would accurately predict relapses.”
The Study Details
The study included patients diagnosed with initial-onset or relapsing granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA) from November 2012–November 2013 who were in complete remission following induction. Of those 162 patients, 117 (72.2%) were diagnosed with GPA, and 45 (27.8%) were diagnosed with MPA.
Patients in this open-label, multicenter trial were randomized to either tailored (n=81) or control (n=81) groups. Controls received a fixed dose of rituximab infusion at Days 0 and 14 following randomization, then at six, 12 and 18 months after the first doses. The tailored patients received the same dose at randomization with reinfusion only when the CD19+ lymphocytes or ANCA reappeared, or ANCA titer rose markedly based on trimestrial testing.

Prof. Guillevin
The patients received intravenous methylprednisolone (100 mg), dexchlorpheniramine (5 mg) and acetaminophen (1,000 mg) before all rituximab infusions. Most were taking low-dose prednisone at randomization, which could be tapered and stopped or maintained at 5 mg/day at the discretion of the site investigator.
Statistical analysis was performed on an intention-to-treat basis. Study visits occurred at enrollment and then every three months until the endpoint, 28 months following randomization. At each visit, a Birmingham Vasculitis Activity Score (BVAS) was calculated. Patients were asked to record their study medication(s) in a weekly diary. ANCA testing and CD19+ B cell counts for a given patient were always determined in the same laboratory.
The primary endpoint was the number of relapses (defined as new, reappearing symptom[s] or a worsening BVAS) at Month 28, as judged by an independent adjudication committee. The committee was blinded to treatment group.
The tailored-infusion arm received 248 infusions compared with 381 in the scheduled group.
Relapses at Month 28
At Month 28, 21 patients had suffered 22 relapses. Of these, 13 patients with 14 relapses (17.3% of the group) were in the tailored-infusion group, and eight people suffered eight (9.9%) relapses in the scheduled-infusion population (P=0.22). Comparing secondary endpoint of relapses, tailored vs. fixed-schedule relapse-free survival rates were 83.8% (95% confidence interval [95% CI] 76.1% to 92.3%) vs. 86.4% (95% CI 79.2 to 94.2) (P=0.58). Major relapses occurred in six (7.4%) vs. three (3.7%) patients (P=0.23).
Glucocorticoid dose and duration did not differ significantly. Twenty-five patients stopped glucocorticoids during the study, but discontinuation was not associated with relapse.
The authors noted the study’s strengths include the fact that it was a multicenter trial using a reinfusion-decision algorithm applied to the experimental arm. The study’s limitations include its open-label nature, the fact that biological parameters were assayed in each center instead of a central laboratory and the fact that interassay variability was not evaluated prior to the study starting.
The Takeaways
Dr. Charles
According to study author Pierre Charles of the Department of Internal Medicine at Institut Mutualiste Montsouris in Paris, “This strategy did not lead to a statistically significant difference in the number of relapses even with the fewer infusions.”
The tailored-infusion arm received 248 infusions compared with 381 in the scheduled group. The medians (interquartile range) were three (ranging from two to four) vs. five (all received five), respectively.
“Fewer infusions were needed when using the individually tailored strategy of rituximab re-administration based on ANCA and circulating CD19+ B cells,” says Dr. Charles. “Although ANCA evolution and/or circulating CD19+ B cells were not reliable predictors of relapse, combining them still achieved fewer infusions in the tailored-infusion arm without significantly more relapses.”
“There are three important takeaways from our study,” says Prof. Guillevin. “Rituximab is the best treatment to maintain AAV remission, a reinfusion strategy based on ANCA and circulating CD19+ B cells could be used to reduce the number of needed rituximab infusions, and ANCA positivity and/or presence of circulating B cells are not useful in predicting relapse in these patients.”
Angelo L. Gaffo, MD, MsPH, is associate professor in the Rheumatology Division at the University of Alabama, Birmingham. He says this is a well-done study by a group with a very good track record in research-related AAV.
“The question on how to use rituximab to maintain remission is still pretty much unanswered,” he says. “This study gives us guidance on how to not only use rituximab as a maintenance drug, but also what role ANCA antibody and CD19+ B cell testing can have in decision making in cases of vasculitis. This is a major contribution because until now there were no known studies that have explored this situation with such rigor.”
Dr. Gaffo
Dr. Gaffo did express some concerns. Because of the pragmatic nature of the study, a few imbalances occurred in the randomization assignments. In addition, “There may be some controversy because the 500 mg of rituximab dosing strategy they chose may not be representative of what everyone does,” he says. “Many centers use a 1,000 mg dose protocol.”
One of the messages for everyday practice is that maintenance strategies for rituximab continue to prove quite effective. They probably should be preferred over regimens that prescribe traditional agents, he says.
“The second important lesson is that basing maintenance strategies on monitoring ANCA and/or CD19+ B cells is a promising method to expose patients to less drug,” said Dr. Gaffo. “This in turn could decrease the cost of treatment while also keeping up effectiveness and keeping patients in remission.”
Kurt Ullman has been a freelance writer for more than 30 years and a contributing writer to The Rheumatologist for more than 10 years.
Does Rituximab Beat Azathioprine?
MAINRITSAN2 confirms rituximab is the best treatment to maintain AAV remission, says Dr. Charles.

Dr. Pagnoux
Christian Pagnoux, MD, MPH, MSc, a rheumatologist at Mount Sinai Hospital and associate professor at the University of Toronto in Canada, notes that an earlier study by the same group in 2014 showed rituximab was superior to conventional maintenance treatment with azathioprine at preventing relapses of patients with GPA or MPA, but rituximab does not have regulatory approval for maintenance in those rare diseases.2
For now, most patients are left with conventional maintenance treatments with azathioprine or methotrexate after remission, says Dr. Pagnoux, who was involved in the first, but not this second, MAINRITSAN trial. “Some [patients] have drug coverage plans that allow rituximab for maintenance, or they pay out of pocket to receive rituximab maintenance reinfusions.
“The good (and reassuring) news from MAINRITSAN2 is that those patients can be treated with rituximab 500 mg reinfusions based on their serial ANCA titers and CD19+ B cell counts, if thoroughly monitored and measured every three months,” Dr. Pagnoux says.
Catherine Kolonko is a medical writer based in Oregon.
References
- Charles P, Terrier B, Perrodeau É, et al. Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: Results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann Rheum Dis. 2018 Aug;77(8):1143–1149.
- Pugnet G, Pagnoux C, Terrier B, et al. Rituximab versus azathioprine for ANCA-associated vasculitis maintenance therapy: Impact on global disability and health-related quality of life. Clin Exp Rheumatol. 2016 May–Jun;34(3 Suppl 97):S54–S59.