NEW YORK (Reuters Health)—The route of iron replacement therapy alters the gut microbiome and metabolomics in patients with inflammatory bowel disease (IBD), but the route is unrelated to disease activity and quality of life, according to a new study.
“Crohn’s disease patients are extremely fragile to disturbances and one might speculate about consequences in long-term disease development,” Dr. Dirk Haller, of the Technical University of Munich, Germany, told Reuters Health by email.
“The sample size is small and because of the heterogeneity in disease phenotype we cannot claim much about the regulation of disease activity,” he added. However, he speculated, “If iron replacement therapy is required, one has to keep in mind that microbiota alterations occur and adjunct bacteriotherapy, such as probiotics, may be indicated.”
The research team conducted an open-label, clinical trial that compared the effects of oral vs. intravenous iron replacement therapy (IRT) on the gut microbiome and metabolite milieu. Seventy-two patients were recruited from gastroenterology ambulatory care practices in Edmonton, Canada (University of Alberta Hospital, Royal Alexandra Hospital), and all completed the study.
Thirty-one patients had Crohn’s disease, 22 had ulcerative colitis, and 19 patients were controls with noninflamed iron deficiency anemia. Patients were randomized 1:1 to receive oral or intravenous iron supplementation, which they took for three months.
The researchers measured pre- and post-iron levels. Fecal bacteria communities and metabolomics were analyzed using high-throughput sequencing and high-resolution mass spectrometry.
Clinical disease activity index and C reactive protein were used to evaluate IRT effect on IBD activity. Iron changes were assessed with serum hemoglobin, ferritin, and iron saturation. Stool samples were analyzed at three and 12 months after treatment.
Iron saturation rates were no different no matter the route of administration, measuring 23.3 in the patients receiving it orally versus 23.9 for the intravenous group, the researchers report in the journal Gut, online on Feb. 4.
Average iron saturation rates reached and hemoglobin levels were also similar at three months. The route of iron replacement did not have any impact on clinical disease activity measures and serum CRP.
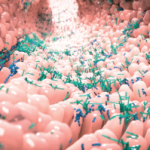
Analyses of specific fecal microbiome fingerprints differentiated Crohn’s disease patients most clearly, with a marked decline in taxa richness and a median effective count <15 species. The most common taxonomic groups were Firmicutes, followed by Actinobacteria, and Bacteroidetes. Metabolome analyses differentiated both patients with ulcerative colitis and Crohn’s disease from controls. Oral administration was linked to decreased Faecalibacterium prausnitzii, Ruminococcus bromii, Dorea Sp., and Collinsella aerofaciens.
Dr. Alan C. Moss, of Harvard Medical School and Beth Israel Deaconess Medical Center, Boston, told Reuters Health by email, “It is of interest that disease activity and quality of life did not differ between type of iron, as older studies reported worsening symptoms with (oral) iron in patients with Crohn’s disease. This may have represented a response to alterations in the microbiome, not inflammation.”
He added, “The microbial and metabolomics data should be considered exploratory, given the small sample size. The noted reductions in Faecalibacterium prausnitzii on (oral) iron did not seem to translate to clinically meaningful differences in disease activity in the short term, which is reassuring.” Dr. Moss also noted that the similar effects of intravenous and oral iron are consistent with previous studies.
The authors reported no funding or disclosures.