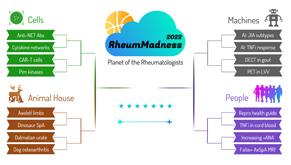
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
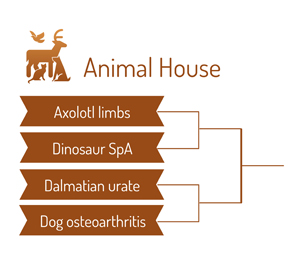
Region: Animal House Team: Dog Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis. Approximately 300 million people worldwide are affected by hip and knee OA.1 OAis associated with significant morbidy, disability and decreased quality of life. It’s no secret: We need better treatment options for OA. Currently, no U.S. Food & Drug Administration-approved disease-modifying drugs exist for OA, and managing symptoms remains the mainstay of therapy.
So how do we improve our research efforts and search for a cure for OA? We may be able to turn to our loyal friend and companion: the dog.
 Dog OA shares a close resemblance to human OA, and treatments are often similar. Dogs and humans have similarities in anatomy, disease heterogeneity and OA progression. They also may share lifestyle, environmental and comorbid conditions (e.g., obesity) along with similar spontaneous diseases, such as hip dysplasia and cruciate ligament rupture, that result in OA. Dog models share more histopathology and pathogenesis factors with human OA than murine models. Example: Changes in articular cartilage proteoglycans are similar in the natural slow development of dog and human OA, but differ from experimentally induced OA.2 Accordingly, this finding may make dogs a better model for OA research than murine models.
Dog OA shares a close resemblance to human OA, and treatments are often similar. Dogs and humans have similarities in anatomy, disease heterogeneity and OA progression. They also may share lifestyle, environmental and comorbid conditions (e.g., obesity) along with similar spontaneous diseases, such as hip dysplasia and cruciate ligament rupture, that result in OA. Dog models share more histopathology and pathogenesis factors with human OA than murine models. Example: Changes in articular cartilage proteoglycans are similar in the natural slow development of dog and human OA, but differ from experimentally induced OA.2 Accordingly, this finding may make dogs a better model for OA research than murine models.
Wait, you want to do research on my best friend?
Studies using naturally occurring forms of dog OA may actually lead to an overall reduction in the number of animals used for experimental research and to a greater understanding of spontaneous OA.
How can we improve basic and clinical research in OA?
- Adopt a one-medicine approach: Collaboration with veterinary researchers can provide tissue samples from early-stage OA and opportunities to evaluate new therapies in dog models of OA. This approach may help develop our understanding and treatment of dog OA, which may further lead to discoveries in human OA.
- Follow veterinary randomized controlled trials (V-RCTs): In companion dogs with OA and chronic pain, V-RCTs may reliably predict treatment efficacy in humans.3,4 A database is currently being developed by the American Veterinary Medical Association, as well as national repositories of dog OA tissue samples and national retrieval banks for implants along with V-RCT guidelines.
Implications
Technological advancements in V-RCTs for dog OA include telemetric accelerometry, the ability to monitor dog locomotion and quantitative sensory testing, the measurement of pain in dogs using temperature or vibration.5 These instruments have the potential to measure improvement in dogs’ functional status after experimental therapies for OA, including orthopedic devices and new medications. It’s easy to imagine that data from these types of trials may be used to predict safety and efficacy of new therapies in humans.
Interestingly, dog OA trials have shown that allogeneic mesenchymal stem cells harvested from adipose tissue can be combined with hyaluronan and injected into the elbows and hips of dogs, resulting in reduced lameness, as well as regeneration of cartilage at these sites.6 Research on the use of stem cells for cartilage regeneration in humans, which is in its early stages, may benefit from the knowledge gained through stem cell trials performed in dogs.
Could a collaboration between veterinary and human researchers accelerate research on stem cell therapies in human OA? This seems like a winning strategy.
Chances in the Tournament
We predict Dog OA will be top dog for the Animal House Region, but this team will face some stiff competition moving forward in the tournament.
A condition with such immense global disease burden and disability deserves high-quality basic and clinical research studies to further understand the pathogenesis of OA. We hope the one-medicine approach and V-RCTs may lead to development of novel therapeutic options and potentially a cure for OA. It appears one way to accomplish this goal is a joint effort between humans and their furry loyal companions.
Nina Couette, DO, is a second-year rheumatology fellow in the Ohio State University Rheumatology Fellowship Program, Columbus, Ohio.
Jesse Reisner, DO, is a first-year rheumatology fellow in the Ohio State University Rheumatology Fellowship Program, Columbus, Ohio.
Sheryl Mascarenhas, MD, is an attending rheumatologist and the fellowship program director of the Ohio State University Rheumatology Fellowship Program, Columbus, Ohio.
References
- Global Health Data Exchange: http://ghdx.healthdata.org/gbd-results-tool.
- Liu W, Burton-Wurster N, Glant TT, et al. Spontaneous and experimental osteoarthritis in dog: Similarities and differences in proteoglycan levels. J Orthop Res. 2003 Jul;21(4):730–737.
- Brown, DC, Boston RC, Coyne JC, et al. Ability of the canine brief pain inventory to detect response to treatment in dogs with osteoarthritis. J Am Vet Med Assoc. 2008 Oct 15;233(8):1278–1283.
- Lascelles BDX, Knazovicky D, Case B, et al. A canine-specific anti-nerve growth factor antibody alleviates pain and improves mobility and function in dogs with degenerative joint disease-associated pain. BMC Vet Res. 2015 Apr 30;11:101.
- Meeson RL, et al. Spontaneous dog osteoarthritis—a one medicine vision. Nat Rev Rheumatol. 2019 May;15(5):273–287.
- Kriston-Pál É, Czibula A, Gyuris Z, et al. Characterization and therapeutic application of canine adipose mesenchymal stem cells to treat elbow osteoarthritis. Can J Vet Res. 2017 Jan;81(1):73–78.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.



