The initial workup could also include blood cultures and a lumbar puncture for cerebrospinal fluid (CSF) studies to rule out infectious etiologies of neurological disease. Remember, it’s not safe to perform a lumbar puncture in the patient with headache and neurological abnormalities without initial neuroimaging for risk of provoking herniation from abrupt changes in intracranial pressure.
Last, but not least, lab testing should include markers of SLE activity (e.g., dsDNA, complement activity or level, erythrocyte sedimentation rate [ESR], C-reactive protein [CRP]) as well as antiphospholipid antibody testing, even if prior hypercoagulability testing has been negative.
Back to the Case
In rheumatology, a patient’s verbal description of their symptoms and triggers carries great importance, and this is no less true when patients present with neurological symptoms. In this case, with the patient intubated and deeply sedated, we were not able to gather any such information from the patient herself. Fortunately, her mother recalled that the patient had been moderately hypertensive (i.e., systolic BPs as high as the 170s) for several days prior to the seizures and that she had noted a visual disturbance in the form of “a rainbow of colors” immediately before her first seizure.
Labs revealed a serum creatinine at a baseline level of 0.63 mg/dL, stable blood cell and platelet counts, and no antiphospholipid antibodies. Her dsDNA was >1,000 international units, which is her baseline, and her complement levels (C3 and C4) were 27 mg/dL and 4 mg/dL, respectively, compared with her usual levels of 60 mg/dL and 10 mg/dL. ESR and CRP were 16 mm/hour and 6 mg/L, respectively.
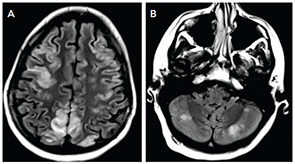
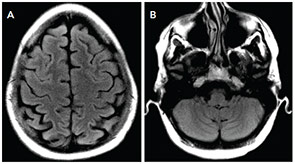
The MRI of the brain showed cortical and subcortical T2 hyperintensities primarily involving bilateral parietal, occipital and posterior temporal lobes (see Figure 1). T2 hyperintense lesions were also seen in the subcortical frontal lobe and bilateral cerebellar hemispheres. There was no evidence of acute ischemic infarct. Lumbar puncture showed three white blood cells, 2,800 red blood cells, glucose of 41 mg/dL and protein of 31 mg/dL. The history of headache, seizure and visual disturbance combined with the MRI findings and noninflammatory CSF are most consistent with posterior reversible encephalopathy syndrome. Levetiracetam for seizure prevention was started, and BP was controlled to systolic of less than 140 mmHg. Over the next three days, her mental status improved to baseline, the headache resolved, and she did not have further seizures or visual disturbances.
