Drop-Seq & the Problem of Specificity
Everything we have discussed up to this point has to do with autoantibody discovery. But if we want to learn more about the cause of disease, we must look at the transcriptome.
If DNA can be thought of as the Book of Life, then RNA represents the words read off the page. As anyone who studied biology in college can tell you, DNA produces messenger RNA, which serves as the template for the production of proteins. The transcriptome is the sum total of all messenger RNAs expressed by an organism. Characterizing the transcriptome—and how the transcriptome changes in the journey from health to illness—may be key to understanding human disease.7
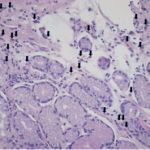
Easier said than done. Consider the kidney, for example. Let’s say that you are enrolled in a biology seminar, and for your final exam, I ask you to propose an experiment to learn more about glomerulonephritis. You may propose to take a kidney biopsy and look at the transcriptome to determine how inflammation changes the proteins expressed by the kidney.
Unfortunately, that may not be good enough. Every kidney biopsy actually consists of multiple cells—endothelium, epithelium, leukocytes, stromal cells—each of which expresses the proteins that serve its needs. What you really would want is to be able to analyze the transcriptome of every cell, individually.
Enter Drop-seq.
First, I should admit that Drop-seq has nothing to do with PhIP-seq, other than being shorthand for the new generation of multiplexed technologies, which perform hundreds of tests in parallel. These high-throughput screening technologies accelerate discovery by performing multiple assays simultaneously.8 It’s almost like having a hundred grad students in your lab, each of whom is performing a slightly different version of the same experiment all at the same time.
With Drop-seq, every cell from a tissue sample is placed in a bubble of fluid, which serves as a miniature lab for that single cell. Using this technique, Steven A. McCarroll’s lab was able to analyze the transcriptome of over 44,000 mouse retinal cells, and identified 39 distinct populations.9 Of these populations, you could imagine that some are vital to our understanding of disease states, and some of them are completely irrelevant. But at least now we have a fighting chance of telling them apart.
Just like PhIP-seq opens new doors for autoantibody discovery, single-cell genomics, transcriptomics (like Drop-seq) and proteomics may open new doors for drug discovery. The Accelerating Medicines Partnership (AMP) is betting big on this. Created in 2014, it is a consortium that includes the NIH, the FDA and multiple pharmaceutical and nonprofit organizations. The consortium recognizes the future of drug discovery lies in developing more efficient ways of determining how novel compounds affect the cells they target. They note:
The entire biomedical research community and the public have a shared interest in compressing the timelines, reducing the costs, and increasing the success rates of new targeted therapies. Given the amount and complexity of the data, this goal will require a systematic approach in which government, academia, industry, and patient groups work collaboratively to sift through the flood of disease targets and find the ones most likely to prove responsive to treatments.10
I think I’m starting to understand why these technologies have so many people so excited. Thinking back to the symposium I attended, it is easy to see how Drop-seq, for example, would be invaluable to expanding our understanding of hypereosinophilic disorders. It would allow us to see the difference in the transcriptome of eosinophils from a patient with eosinophilic granulomatosis with polyangiitis, and compare it to the transcriptome of a patient with allergic sinusitis or eosinophilic colitis. We would finally have a way of understanding these diseases that is more sophisticated than counting the number of eosinophils that appear on a microscope slide. Similarly, PhIP-seq could be used to identify novel autoantibodies that drive all of these diseases.
These are not the only seq technologies that are changing the landscape of discovery. There are also Epi-seq, CEL-seq2, MAUI-seq, ChIP-seq, Perturb-seq and others, each of which takes an older technology and makes it work faster. All of these technologies will likely change how we think about many of our diseases, making connections we don’t even know we should be looking for. Of course, these technologies come with barriers of their own: The cost of these technologies is enormous, and analyzing their output is beyond complicated. That said, up until now, research has depended on our asking questions that were answerable. Increasingly, we are now able to ask the questions we really want answered and follow the data wherever they lead.