In the past, when treatment options were limited, the natural history of RA involved severe outcomes in both men and women over the course of disease of five to 20 years.13 Severe long-term outcomes of RA were reported equally in women and men in terms of clinical disease activity, structural damage, and deformities.14-19 At present, the health status of RA patients is significantly better compared with that observed in previous decades, according to a variety of measures including disease activity, function and structural outcomes, work disability, and mortality rates.20-30 Importantly, these measures do not show a sex preference. Nonetheless, as in the general population, men with RA have considerably higher mortality rates than women.31
Gathering Data on Sex Differences and RA
What, therefore, accounts for the sudden change in the view that RA is worse in women than in men? With this question in mind, my colleagues and I sought to analyze in our research the possible influence of sex differences on the clinical status and course of RA in a large, multinational, clinical RA database.32
The Quantitative Standard Monitoring of Patients with RA (QUEST-RA) program was established in 2005 to promote quantitative assessment in usual clinical care at multiple sites and to develop a database of RA patients seen outside of clinical trials in usual care in many countries.19 Data collection began in January 2005; by July 2009, the program had expanded to include 8,039 patients from 86 sites in 32 countries.
This study was designed to reflect good clinical practice. Rheumatologists performed a clinical review of each patient, and patients completed a four-page self-report questionnaire. Sex differences were analyzed for the measures of disease activity according to the RA core data set measures, disease-activity score (DAS28), fatigue; clinical characteristics such as the presence of rheumatoid factor, nodules and erosion; and for the current use of diseasemodifying drugs including prednisone, methotrexate, and biologic agents.
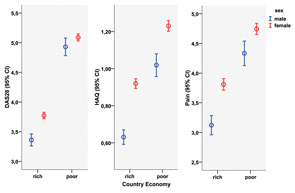
Results of QUEST-RA confirmed other reports that women had poorer scores than men in all core data set measures, including the number of swollen joints (4.5 swollen joints in women versus 3.8 in men) and tender joints (6.9 versus 5.4, respectively), both on a 28-joint count; erythrocyte sedimentation rate (30 mm/h versus 26 mm/h); functional status on the health assessment questionnaire (HAQ) (1.1 versus 0.8); visual analog scales for physician global estimate (3.0 versus 2.5), pain (4.3 versus 3.6), patient global estimate of status (4.2 versus 3.7), and fatigue (4.6 versus 3.7); and DAS28 (4.3 versus 3.8) (p<0.001 for all comparisons).33 Differences in clinical variables between sexes were seen in rich and poor countries (see Figure 1, above), expanding our previous observations that RA disease activity in each country and gross domestic product have a strong negative association among countries.34
