During the past few years, there has been increasing interest in the proposition that, when it comes to rheumatoid arthritis (RA), sex really matters. Suddenly, articles on sex and gender differences in RA abound in the scientific literature as well as the lay press. Most importantly, these articles advance the idea that the course of RA is significantly worse in women when compared with men.
The implications of this idea are profound and affect both clinical care and scientific research. This view that RA is worse in women than in men may seem surprising to clinical rheumatologists who have seen progressive disability in patients of both sexes. Correspondingly, clinical rheumatologists have seen impressive treatment responses and also spontaneous remissions in men as well as women. Nevertheless, news about differences between women and men in the course of disease seems “hot” and inevitably attracts fanfare and attention. As this review will argue, it should also attract careful scrutiny and perhaps skepticism.
Not surprisingly, reports indicating differences in the course and outcomes of RA according to sex (as well as other unexpected influences) appear to gain more attention than reports indicating the absence of an effect. Ten years ago, a study from the Mayo Clinic compared 55 male patients to 110 female patients with a similar disease duration of at least 10 years.1 This study showed that erosive disease was more prevalent and developed earlier in men than in women. The investigators suggested that this finding, along with others in the study, might help “assess the prognosis and tailor the treatment of the individual patient.” This suggestion was seen by some members of the rheumatology community as a reflection of an old-fashioned treatment approach of “go low, go slow” that should be abandoned. A modern treatment strategy with early and aggressive therapies was suggested to apply equally both sexes.2
By contrast, male sex was recently shown to be a major predictor of remission in early RA.3,4 Analyses of RA differences include studies indicating higher disease activity and poorer functional status in women when compared with men.3–7 Some recent studies have also suggested that men have better responses to treatment with biologic agents than women.5–7 On the other hand, men have been shown to experience more adverse effects, particularly serious infections, during biologic treatments.8,9
There are obvious differences between the sexes concerning the prevalence, age at onset, and autoantibody production in RA.10 The prevalence of RA differs between sexes, primarily among menstruating women. Although the majority of patients with RA are middle-aged women, generally greater than 70% in any RA cohort, RA can nonetheless occur at any age in both sexes. Furthermore, sex differences are seen in biologic factors (e.g., hormones) or behavioral factors (e.g., smoking) that may influence susceptibility to and the phenotype of RA.11,12
In the past, when treatment options were limited, the natural history of RA involved severe outcomes in both men and women over the course of disease of five to 20 years.13 Severe long-term outcomes of RA were reported equally in women and men in terms of clinical disease activity, structural damage, and deformities.14-19 At present, the health status of RA patients is significantly better compared with that observed in previous decades, according to a variety of measures including disease activity, function and structural outcomes, work disability, and mortality rates.20-30 Importantly, these measures do not show a sex preference. Nonetheless, as in the general population, men with RA have considerably higher mortality rates than women.31
Gathering Data on Sex Differences and RA
What, therefore, accounts for the sudden change in the view that RA is worse in women than in men? With this question in mind, my colleagues and I sought to analyze in our research the possible influence of sex differences on the clinical status and course of RA in a large, multinational, clinical RA database.32
The Quantitative Standard Monitoring of Patients with RA (QUEST-RA) program was established in 2005 to promote quantitative assessment in usual clinical care at multiple sites and to develop a database of RA patients seen outside of clinical trials in usual care in many countries.19 Data collection began in January 2005; by July 2009, the program had expanded to include 8,039 patients from 86 sites in 32 countries.
This study was designed to reflect good clinical practice. Rheumatologists performed a clinical review of each patient, and patients completed a four-page self-report questionnaire. Sex differences were analyzed for the measures of disease activity according to the RA core data set measures, disease-activity score (DAS28), fatigue; clinical characteristics such as the presence of rheumatoid factor, nodules and erosion; and for the current use of diseasemodifying drugs including prednisone, methotrexate, and biologic agents.
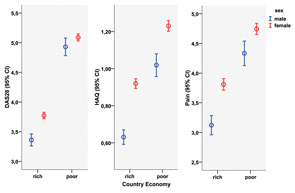
Results of QUEST-RA confirmed other reports that women had poorer scores than men in all core data set measures, including the number of swollen joints (4.5 swollen joints in women versus 3.8 in men) and tender joints (6.9 versus 5.4, respectively), both on a 28-joint count; erythrocyte sedimentation rate (30 mm/h versus 26 mm/h); functional status on the health assessment questionnaire (HAQ) (1.1 versus 0.8); visual analog scales for physician global estimate (3.0 versus 2.5), pain (4.3 versus 3.6), patient global estimate of status (4.2 versus 3.7), and fatigue (4.6 versus 3.7); and DAS28 (4.3 versus 3.8) (p<0.001 for all comparisons).33 Differences in clinical variables between sexes were seen in rich and poor countries (see Figure 1, above), expanding our previous observations that RA disease activity in each country and gross domestic product have a strong negative association among countries.34
Despite statistically significant differences in the values between men and women, the effect sizes of these measures were limited and smallest for the swollen joint count, which was then used as an objective surrogate for inflammation. Among patients who had minimal disease activity in terms of joint swelling (i.e., no swollen joints or only one), women had statistically significantly higher mean values compared with men in all other disease activity measures (p<0.001) and met DAS28 remission criteria less frequently than men.35 Similar proportions of females and males were taking the various therapies. Rheumatoid factor was equally prevalent among genders. Men had nodules more often than women. Women had erosions more often than men, but the statistical significance was marginal, echoing data from other studies with similar radiographic progression in women and men.36–38
The QUEST-RA data show that currently used disease-activity measures indicate higher activity in women than in men. The higher likelihood of remission in men versus women according to DAS28 can be explained in large part by the observation that higher values for all DAS28 components were seen in women.33 Indeed, most people over age 50 years in the general population who do not have RA do not meet the ACR remission criteria for RA—women less often than men.39 Disease severity was similar between sexes with respect to the proportion of women and men with an erosive disease; in addition, from what is known about long-term outcomes from longitudinal cohorts, it appears that most gender differences in RA disease activity may result from characteristics of the measures of disease activity, rather than from RA disease activity itself.
Explaining Other Sex Differences
At present, a “gold standard” for RA disease activity does not exist. Furthermore, the currently used disease-activity measures may reflect phenomena other than those associated with RA, which may lead men to have better scores. Several reports indicate that women with RA report more severe symptoms, greater disability, and higher work disability rates compared with men.40-42 Women report poorer scores than men for daily physical activities; this finding is understandable because women have less strength than men.40,41;43–48 In fact, the sex differences in musculoskeletal performance remain even among the most physically fit, best-trained individuals. After all, female and male athletes compete separately.
It is of particular interest that gender differences for DAS28, fatigue, and RA Core Data Set measures were most pronounced in patients with low swollen joint counts in the QUEST-RA study. This finding can be interpreted to suggest that, even at minor disease activity levels, the burden of the disease is greater for women than for men, or that women are more likely than men to report problems. Concerning musculoskeletal size and strength, women’s baseline values are lower than men’s. Therefore, the same severity of a musculoskeletal disease may be reported as a problem more often by women than men.
Considering these factors, language used to describe outcomes in rheumatic disease may need modification as well as a new conceptualization. Thus, the phrase “Male sex—a major predictor of remission” might be more accurately stated as “Male sex—a major predictor of meeting remission criteria.”49 Furthermore, in trying to convey better male–female differences in the course of RA, it is important to consider that disease-activity measures, especially in the setting of low disease activity near remission, behave differently in men than in women; there are nevertheless exceptions.50
Therefore, one may pose the question of whether we need new criteria for remission that treat men and women separately. Certainly, the current criteria sets used for RA remission vary in stringency, thereby affecting the percentage of patients achieving a level of disease activity operationally defined as remission. Among the criteria sets, the level of activity defining remission may vary depending on the number of factors assessed, the weighting, and even the number of joints assessed. Therefore, in populations of patients, remission rates have to be interpreted in light of the definition that has been used for remission. In case of an individual patient, however, whether a man or a woman, “we recognize it (remission) when we see it,” according to a wise suggestion by Paulus.51
Data and beliefs exert powerful influences on science and medicine and affect the way we think and the way we act. Rheumatology is no different than other specialties, although, when it comes to the matter of sex, beliefs may have trumped data. From my reading of the data, I would conclude that, despite some differences in the measures of disease activity, RA is essentially the same disease in women and men. Furthermore, anyone who has read this article to this point may conclude that news concerning differences in disease course between women and men, like everything else having to do with sex, can attract attention. Now that I have your attention, I hope that you will look at the data.
Acknowledgement: This article is based in part on data presented in Sokka T, et al. Arthritis Res Ther. 2009; 11(1):R7.
Dr. Sokka is a rheumatologist at the Jyväskylä Central Hospital in Jyväskylä, Finland.
References
- Weyand CM, Schmidt D, Wagner U, Goronzy JJ. The influence of sex on the phenotype of rheumatoid arthritis. Arthritis Rheum. 1998;41:817-822.
- Boers M. Does sex of the rheumatoid arthritis patients matter? Lancet. 1998;352:419-420
- Forslind K, Hafstrom I, Ahlmen M, Svensson B. Sex: A major predictor of remission in early rheumatoid arthritis? Ann Rheum Dis. 2007;66:46-52.
- Mancarella L, Bobbio-Pallavicini F, Ceccarelli F, et al. Good clinical response, remission, and predictors of remission in rheumatoid arthritis patients treated with tumor necrosis factor-alpha blockers: The GISEA study. J Rheumatol. 2007;34:1670-1673.
- Hyrich KL, Watson KD, Silman AJ, Symmons DP, British Society for Rheumatology Biologics Register. Predictors of response to anti-TNF-a therapy among patients with rheumatoid arthritis: Results from the British Society for Rheumatology Biologics Register. Rheumatology (Oxford). 2006;45:1558-1565.
- Yamanaka H, Tanaka Y, Sekiguchi N, et al. Retrospective clinical study on the notable efficacy and related factors of infliximab therapy in a rheumatoid arthritis management group in Japan (RECONFIRM). Mod Rheumatol. 2007;17:28-32.
- Kvien TK, Uhlig T, Odegard S, Heiberg MS. Epidemiological aspects of rheumatoid arthritis: The sex ratio. Ann N Y Acad Sci. 2006;1069:212-222.
- Burmester GR, Mariette X, Montecucco C, et al. Adalimumab alone and in combination with disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis in clinical practice: The Research in Active Rheumatoid Arthritis (ReAct) trial. Ann Rheum Dis. 2007;66:732-739.
- Takeuchi T, Tatsuki Y, Nogami Y, et al. Postmarketing surveillance of the safety profile of infliximab in 5,000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis. 2008;67:189-194.
- Jawaheer D, Lum RF, Gregersen PK, Criswell LA. Influence of male sex on disease phenotype in familial rheumatoid arthritis. Arthritis Rheum. 2006;54:3087-3094.
- Straub RH, Harle P, Sarzi-Puttini P, Cutolo M. Tumor necrosis factor-neutralizing therapies improve altered hormone axes: An alternative mode of antiinflammatory action. Arthritis Rheum. 2006;54:2039-2046.
- Krishnan E, Sokka T, Hannonen P. Smoking-gender interaction and risk for rheumatoid arthritis. Arthritis Res Ther. 2003;5:R158-R162.
- Jantti JK, Kaarela K, Belt EA, Kautiainen HJ. Incidence of severe outcome in rheumatoid arthritis during 20 years. J Rheumatol. 2002;29:688-692.
- Yelin E, Meenan R, Nevitt M, Epstein W. Work disability in rheumatoid arthritis: Effects of disease, social, and work factors. Ann Intern Med. 1980;93:551-556.
- Mäkisara GL, Mäkisara P. Prognosis of functional capacity and work capacity in rheumatoid arthritis. Clin Rheumatol. 1982;1:117-125.
- Scott DL, Grindulis KA, Struthers GR, et al. Progression of radiological changes in rheumatoid arthritis. Ann Rheum Dis. 1984;43:8-17.
- Pincus T, Callahan LF, Sale WG, et al. Severe functional declines, work disability, and increased mortality in seventy-five rheumatoid arthritis patients studied over nine years. Arthritis Rheum. 1984;27:864-872.
- Kaarela K. Prognostic factors and diagnostic criteria in early rheumatoid arthritis. Scand J Rheumatol Suppl. 1985;57:1-54.
- Sokka T, Kautiainen H, Toloza S, et al. QUEST-RA: quantitative clinical assessment of patients with rheumatoid arthritis seen in standard rheumatology care in 15 countries. Ann Rheum Dis. 2007;66:1491-1496.
- Bergstrom U, Book C, Lindroth Y, et al. Lower disease activity and disability in Swedish patients with rheumatoid arthritis in 1995 compared with 1978. Scand J Rheumatol. 1999;28:160-165.
- Pincus T, Sokka T, Kautiainen H. Patients seen for standard rheumatoid arthritis care have significantly better articular, radiographic, laboratory, and functional status in 2000 than in 1985. Arthritis Rheum. 2005;52:1009-1019.
- Sokka T, Möttönen T, Hannonen P. Disease-modifying anti-rheumatic drug use according to the “sawtooth” treatment strategy improves the functional outcome in rheumatoid arthritis: Results of a long-term follow-up study with review of the literature. Rheumatology. 2000;39:34-42.
- Krishnan E, Fries JF. Reduction in long-term functional disability in rheumatoid arthritis from 1977 to 1998: A longitudinal study of 3035 patients. Am J Med. 2003;115:371-376.
- Heiberg T, Finset A, Uhlig T, Kvien TK. Seven year changes in health status and priorities for improvement of health in patients with rheumatoid arthritis. Ann Rheum Dis. 2005; 64:191-195.
- Sokka TM, Kaarela K, Möttönen TT, Hannonen PJ. Conventional monotherapy compared to a “sawtooth” treatment strategy in the radiographic procession of rheumatoid arthritis over the first eight years. Clin Exp Rheumatol. 1999;17:527-532.
- Sokka T, Kautiainen H, Häkkinen K, Hannonen P. Radiographic progression is getting milder in patients with early rheumatoid arthritis. Results of 3 cohorts over 5 years. J Rheumatol. 2004;31:1073-1082.
- Sokka T, Kautiainen H, Hannonen P. Stable occurrence of knee and hip total joint replacement in Central Finland between 1986 and 2003: An indication of improved long-term outcomes of rheumatoid arthritis. Ann Rheum Dis. 2007;66:341-344.
- 28. Puolakka K, Kautiainen H, Möttönen T, et al. Early suppression of disease activity is essential for maintenance of work capacity in patients with recent-onset rheumatoid arthritis: Five-year experience from the FIN-RACo trial. Arthritis Rheum. 2005;52:36-41.
- Krause D, Schleusser B, Herborn G, Rau R. Response to methotrexate treatment is associated with reduced mortality in patients with severe rheumatoid arthritis. Arthritis Rheum. 2000;43:14-21.
- Choi HK, Hernán MA, Seeger JD, Robins JM, Wolfe F. Methotrexate and mortality in patients with rheumatoid arthritis: a prospective study. Lancet. 2002;359:1173-1177.
- Isomäki HA. Mortality in Patients with Rheumatoid Arthritis. In: Wolfe F, Pincus T, eds. Rheumatoid Arthritis: Pathogenesis, Assessment, Outcome, and Treatment. New York: Marcel Dekker, Inc.; 1994:235-246.
- Sokka T, Toloza S, Cutolo M, et al. Women, men, and rheumatoid arthritis: Analyses of disease activity, disease characteristics, and treatments in the QUEST-RA Study. Arthritis Res Ther. 2009;11(1):R7.
- Leeb BF, Haindl PM, Maktari A, Nothnagl T, Rintelen B. Disease activity score-28 values differ considerably depending on patient’s pain perception and sex. J Rheumatol. 2007; 34:2382-2387.
- Sokka T, Kautiainen H, Pincus T, et al. Disparities in rheumatoid arthritis disease activity according to gross domestic product in 25 countries in the QUEST-RA database. Ann Rheum Dis. 2009 July 31 (Epub ahead of print).
- Sokka T, Hetland ML, Makinen H, et al. Remission and rheumatoid arthritis: Data on patients receiving usual care in twenty-four countries. Arthritis Rheum. 2008;58:2642-2651.
- Luukkainen R, Kaarela K, Isomäki H, et al. The prediction of radiological destruction during the early stage of rheumatoid arthritis. Clin Exp Rheumatol. 1983;1:295-298.
- Ahlmen M, Svensson B, Albertsson K, Forslind K, Hafstrom I. Influence of gender on assessments of disease activity and function in early rheumatoid arthritis in relation to radiographic joint damage. Ann Rheum Dis. 2009 Jan 21 (Epub ahead of print).
- Gossec L, Baro-Riba J, Bozonnat MC, et al. Influence of sex on disease severity in patients with rheumatoid arthritis. J Rheumatol. 2005;32:1448-1451.
- Sokka T, Makinen H, Hannonen P, Pincus T. Most people over age 50 in the general population do not meet ACR remission criteria or OMERACT minimal disease activity criteria for rheumatoid arthritis. Rheumatology (Oxford). 2007;46:1020-1023.
- Katz PP, Criswell LA. Differences in symptom reports between men and women with rheumatoid arthritis. Arthritis Care Res. 1996;9:441-448.
- Sherrer YS, Bloch DA, Mitchell DM, et al. Disability in rheumatoid arthritis: Comparison of prognostic factors across three populations. J Rheumatol. 1987;14:705-709.
- Puolakka K, Kautiainen H, Pekurinen M, et al. Monetary value of lost productivity over a 5-year follow up in early rheumatoid arthritis estimated on the basis of official register data on patients’ sickness absence and gross income: Experience from the FIN-RACo Trial. Ann Rheum Dis. 2006;65:899-904.
- Thompson PW, Pegley FS. A comparison of disability measured by the Stanford Health Assessment Questionnaire disability scales (HAQ) in male and female rheumatoid outpatients. Br J Rheumatol. 1991;30:298-300.
- McKenna F, Tracey A, Hayes J. Assessment of disability in male and female rheumatoid patients. Br J Rheumatol. 1991;30:477.
- Sokka T, Krishnan E, Häkkinen A, Hannonen P. Functional disability in rheumatoid arthritis patients compared with a community population in Finland. Arthritis Rheum. 2003; 48:59-63.
- Krishnan E, Sokka T, Hakkinen A, Hubert H, Hannonen P. Normative values for the Health Assessment Questionnaire disability index: Benchmarking disability in the general population. Arthritis Rheum. 2004;50:953-960.
- Hakkinen A, Kautiainen H, Hannonen P, et al. Muscle strength, pain, and disease activity explain individual subdimensions of the health assessment questionnaire disability index, especially in women with rheumatoid arthritis. Ann Rheum Dis. 2006;65:30-34.
- Hallert E, Thyberg I, Hass U, Skargren E, Skogh T. Comparison between women and men with recent onset rheumatoid arthritis of disease activity and functional disability over two years (the TIRA project). Ann Rheum Dis. 2003;62:667-670.
- Makinen H, Hannonen P, Sokka T. Sex: A major predictor of remission as measured by 28-joint Disease Activity Score (DAS28) in early rheumatoid arthritis? Ann Rheum Dis. 2008;67:1052-1053.
- Radovits BJ, Fransen J, van Riel PL, Laan RF. Influence of age and gender on the Disease Activity Score-28 (DAS28) in rheumatoid arthritis. Ann Rheum Dis. 2008;67:1127-1131.
- Paulus HE. Defining remission in rheumatoid arthritis: What is it? Does it matter? J Rheumatol. 2004;31:1-4.
