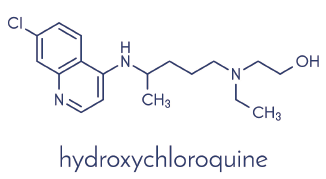
The Johns Hopkins Lupus Center, Baltimore, has described its experience using hydroxychloroquine (HCQ) levels.1 Forty-four percent of its patients had levels below 500 ng/mL (partial nonadherence); 13% were severely nonadherent (<200 ng/mL). They were shown their results and educated on HCQ adherence. Adherence then improved to 80%; those with lower HCQ levels had higher disease activity.
Per the treat-to-target recommendations for lupus, I aim for remission or low disease activity.2 Checking HCQ levels appeared to be an easy way to reduce disease activity and decrease the need for additional immunosuppressant medications. Therefore, I began to check HCQ levels in all patients not in remission.
I found that most who were not in remission did not have therapeutic drug levels; I then discussed these results with each patient. This led to discussions on ways to improve adherence. When my patients realized I was monitoring their levels, adherence rates improved, resulting in better HCQ levels and lower disease activity.
StudioMolekuul / shutterstock.com
Two patients were having repeated flares of their lupus nephritis, with multiple changes in their immunosuppressant therapies plus increased steroid use. Although they told me they were taking their medicines regularly, their HCQ drug levels were undetectable. Their pharmacists confirmed that one had not picked up HCQ in two years and the other in over a year. Both had similar responses when I confronted them: They did not think HCQ was important; it never seemed to make them feel much better when they took it. Following our conversations, both became adherent to their HCQ, resulting in therapeutic levels. Amazingly, both went into remission with these improvements in their levels.
These results (lupus renal remission with HCQ added to immunosuppressant therapy) reminded me of the 2006 Hopkins study that showed adding HCQ to mycophenolate mofetil increased lupus membranous nephritis remission rates three-fold.3
Both patients also admitted they had repeated periods of nonadherence over the years, with recurrent flares of their systemic lupus erythematosus (SLE), resulting in my using more steroids and immunosuppressant therapies. I can’t help but think about what their courses would have been if I could have measured HCQ levels earlier on. If I could have identified their poor adherence earlier, I could have forged better adherence patterns, resulting in fewer flares, less steroid use and fewer immunosuppressants, leading to less permanent organ damage.
I already see the usefulness of HCQ levels in my younger patients. It is common for them to stop their medications, resulting in flares. I catch their poor adherence, discuss the results and reinforce the benefits of taking HCQ; this is followed by better HCQ levels. I am now noting better adherence in these patients compared with my experience with similar patients 10–20 years ago.
I also find HCQ level testing helpful with adjusting doses. I initially prescribe—per the American Academy of Ophthalmology’s (AAO) recommendations—<5 mg/kg of actual body weight.4 In patients who aren’t in remission and who are on doses less than 400 mg a day, if levels are subtherapeutic, I increase their dose.
I find comfort documenting in their records that I am following HCQ levels to achieve better disease control. Although I have not systematically evaluated the results of this practice, many of these patients improve in disease activity. Although the PLUS study was unable to demonstrate decreased lupus flares using HCQ levels to adjust doses, I used HCQ levels and dose adjustments differently, and this deserves study on a larger scale.5 The AAO’s dosing recommendation looked only at the potential for retinopathy, not efficacy. HCQ drug levels and disease activity should be considered in future dosing guidelines.
In my practice, I also have three patients who had undergone gastric bypass surgery (two SLE patients and one with primary Sjögren’s syndrome) and who had subtherapeutic HCQ levels on 400 mg a day. Considering the possibility of HCQ malabsorption, I increased their doses to 500–600 mg a day, resulting in therapeutic drug levels. Two of the three patients went into remission.6
Michelle Petri, MD, MPH, medical director of the Johns Hopkins Lupus Center, showed that patients who had HCQ levels above 1,200 ng/mL were around five times more likely to have HCQ retinopathy.7 “Now that we have shown that HCQ blood levels are predictive of retinopathy,” she says, “I do think there is a rationale for lowering doses in those who are in the highest tertile.”
Nathalie Costedoat-Chalumeau, MD, noted in an editorial that elevated levels are associated with HCQ-induced skin pigmentation and gastrointestinal side effects.8,9 She says it is not unreasonable to lower patients’ doses if levels are >1,500 ng/mL. “I have also been checking HCQ levels in patients who are in remission and lowering their doses if levels are ≥1,500 ng/mL.”
The French have been testing HCQ drug levels for about 15 years. Dr. Costedoat-Chalumeau and colleagues reported their results of HCQ testing in SLE patients in 2006. Seven percent of their patients were severely nonadherent (range 0–129 ng/mL), and whole blood levels of around 1,000 ng/mL were associated with fewer flares of SLE.10
They measure HCQ levels during routine appointments and during SLE flares. Low levels during routine visits identify patients who are poorly adherent and at high risk for flares. This even occurs in their “most charming patients.” They approach patients nonjudgmentally, letting them know it is not uncommon to miss doses. This leads to dialogue exploring the reasons for poor adherence and coming up with solutions.
“A vital part of this discussion is emphasizing to the patient about the importance of taking HCQ regularly and emphasizing the numerous benefits of HCQ,” says Dr. Costedoat-Chalumeau. After thoughtful discussion, the vast majority improve adherence and achieve better disease control.
In flaring lupus patients, such discussions also lead to better adherence, decreasing the use of additional immunosuppressants. In flaring patients who have excellent levels, additional immunomodulatory therapy can be added. Dr. Costedoat-Chalumeau stresses, “The use of HCQ drug levels during flares helps in avoiding unnecessary and potentially dangerous escalations of therapy. The ability to objectively identify HCQ poor adherence and manage patients dependent upon the results has significantly changed the daily management of our SLE patients.”
The data supporting HCQ level testing are overwhelming. Few things in rheumatology prove so helpful in such a large percentage of patients.
“Regularly measuring hydroxychloroquine drug levels should become the standard of care in the management of all patients who have lupus,” says Dr. Petri. “We now recognize that we don’t want patients’ drug levels to be too high or too low. Hydroxychloroquine is our only lupus medication proven to improve survival, and we need to do everything possible to maximize its usage in our patients.” R
Donald E. Thomas, MD, FACP, FACR, is an associate professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Md., and is in private practice at Arthritis and Pain Associates of P.G. County, Greenbelt, Md.
Nathalie Costedoat-Chalumeau, MD, PhD, is a professor of internal medicine at René Descartes University and Cochin Hospital, Paris, France, and is a member of the Systemic Lupus International Collaborating Clinics (SLICC).
Michelle Petri, MD, MPH, is a professor of medicine at the Johns Hopkins University School of Medicine, Baltimore, the director of the Hopkins Lupus Center and a member of the SLICC.
Disclosure: Dr. Thomas is a member of Exagen Diagnostics’ speakers bureau.
References
- Durcan L, Clarke WA, Magder LS, Petri M. Hydroxychloroquine blood levels in systemic lupus erythematosus: Clarifying dosing controversies and improving adherence. J Rheumatol. 2015 Nov;42(11):2092–2097.
- Van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: Recommendations from an international task force. Ann Rheum Dis. 2014 Jun;73(6):958–967.
- Katitanon N, et al. Hydroxychloroquine use predicts complete renal remission within 12 months among patients treated with mycophenolate mofetil therapy for membranous lupus nephritis. Lupus. 2006;15(6):366–370.
- Marmor MF, et al. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology. 2016 Jun;123(6):1386–1394.
- Costedoat-Chalumeau N, Galicier L, Aumaître O, et al. Hydroxychloroquine in systemic lupus erythematosus: Results of a French multicentre controlled trial (PLUS Study). Ann Rheum Dis. 2013 Nov;72(11):1786–1792.
- Thomas DE, et al. Low hydroxychloroquine blood levels in patients who have had gastric bypass surgery. Lupus Sci Med. 2019 Jun;6(1):e000335.
- Petri M, Elkhalifa M, Goldman D, et al. Hydroxychloroquine blood levels show significant trend test for risk for retinopathy [abstract 2897]. Arthritis Rheum. 2018;70(suppl 10).
- Moez J, Francès C, Piette J-C, et al. Hydroxychloroquine-induced pigmentation in patients with systemic lupus erythematosus: A case-control study. JAMA Dermatol. 2013 Aug;149(8):935–940.
- Costedoat-Chalumeau N, Tamirou F, Le Guern V, et al. [Blood concentration of hydroxychloroquine in systemic lupus erythematosus care: Usefulness and limits]. Rev Med Interne. 2017 Feb;38(2):77–80.
- Costedoat-Chalumeau N, Amoura Z, Hulot J-S, et al. Low blood concentration of hydroxychloroquine is a marker for and predictor of disease exacerbations in patients with systemic lupus erythematosus. Arthritis Rheum. 2006 Oct;54(10):3284–3290.


