Zephyr / Science Source
Patients with scleroderma, systemic sclerosis (SSc), myositis and rheumatoid arthritis (RA) may develop interstitial lung disease (ILD), which affects a patient’s breathing and quality of life. Prospective studies have revealed that in patients with SSc a greater rate of decline of forced vital capacity (FVC) is associated with increased mortality. Although corticosteroids are commonly used to treat these patients, little evidence supports this approach. Alternatively, physicians may prescribe cyclophosphamide to treat patients with severe disease and/or rapidly progressing disease even though it is associated with multiple side effects and toxicities.
Cochrane Library Review
A new Cochrane Library review by Hayley Barnes, MBBS, a pulmonologist at Monash University in Australia, and colleagues, evaluated whether cyclophosphamide can help preserve lung function in patients with ILD due to connective tissue disease. The authors also examined whether cyclophosphamide helps improve quality of life, length of life, breathing and ability to exercise, as well as the cost at which the treatment achieves these benefits.1
The team found that patients with ILD associated with connective tissue disease may realize a small benefit from cyclophosphamide treatment. Unfortunately, because connective tissue disease-associated ILD is a rare lung disease, research in this area is challenged by the small number of potential study participants.
Additionally, researchers found a small benefit in terms of % FVC when cyclophosphamide was compared with placebo, but they found no difference in % diffusing capacity of the lung for carbon monoxide (DLCO). They also found modest clinical improvement in dyspnea in patients treated with cyclophosphamide. However, the authors note that in many cases the estimates of effect were imprecise. They found no difference in efficacy when cyclophosphamide was compared with mycophenolate mofetil.
Cyclophosphamide May Benefit Patients—at a Cost
Dr. Barnes and colleagues reviewed studies published prior to May 2017 and identified four studies that included 495 patients with ILD due to connective tissue disease. Three of the studies included only participants with SSc, and one included participants with SSc, dermatomyositis/polymyositis, systemic lupus erythematosus (SLE) and RA. The authors did not perform a separate analysis of the different subgroups. Participants in the studies tended to have relatively stable disease, baseline lung function of 66% to 80% FVC and no recent exacerbations or rescue immunosuppression therapy. Thus, the authors note the evidence presented in their review was derived largely from well participants. Additionally, the studies primarily included patients with SSc. But because it is not clear that evidence of efficacy in one connective tissue disease subtype can be extrapolated to all forms, the authors caution the results may not apply to all patients with ILD with connective tissue disease.
The blind, randomized controlled trials identified in the review included patients given cyclophosphamide, as well as patients prescribed other drugs or placebo. The duration of treatment with cyclophosphamide was limited to 12 months due to concerns of adverse events. One trial found a clinically and statistically significant improvement in breathlessness in patients taking cyclophosphamide compared with controls. In particular, cyclophosphamide appeared to protect against decreased FVC among patients with worse fibrosis scores. Another trial found a statistically significant improvement measure of quality of life in patients treated with cyclophosphamide when compared with placebo controls. However, many participants withdrew from these trials due to adverse events, treatment failure and participant preference. In particular, patients in the cyclophosphamide treatment groups experienced leukopenia, neutropenia, thrombocytopenia, anemia and nausea.
Shervin Assassi, MD, a rheumatologist at McGovern Medical School at the University of Texas Health Science Center, Houston, spoke with The Rheumatologist about the findings. While noting that, in the U.S., mycophenolate is typically prescribed to these patients, he adds, “It is reasonable to ask what the evidence is to support that decision.” Given prescription practices in the U.S., he thinks the two randomized control trials comparing cyclophosphamide with mycophenolate were of greatest interest. One of the trials was written and published in Chinese, and the other is the well-known Scleroderma Lung Study II published in 2016.2
“Both cyclophosphamide and mycophenolate have comparable effects, but mycophenolate is thought to be safer,” Dr. Assassi says. “At this point, we are using mycophenolate based on the results of the 2016 study.”
Call for More Research
The authors concluded the review by suggesting clinical practice guidelines advise clinicians to consider individual patient characteristics when determining treatment. In particular, they suggest that patients with minor or subclinical disease are unlikely to benefit from cyclophosphamide and are likely to experience adverse effects.
Dr. Assassi agrees, noting that “one-third of the patients don’t respond to immunosuppression.” Thus, a great need exists to find biomarkers to identify these patients. The current evidence suggests that histological subtype and disease duration can’t be used to predict responsiveness to treatment.
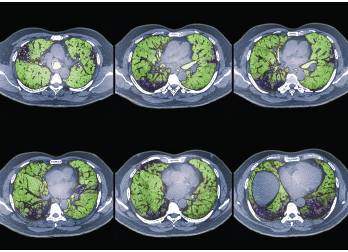
The review described the evidence as low quality due to the limited number of studies in the field. The authors suggest future studies on the use of cyclophosphamide be adequately powered to compare outcomes within different subgroups. They suggest the groups should be large enough to stratify the extent of pulmonary infiltrates as determined by high-resolution computed tomography, as well as skin involvement in patients with SSc. This suggestion is due to the fact that patients with rapidly progressive fibrotic disease may be in the best position to benefit from cyclophosphamide treatment and these patients are not well represented in the current literature. The authors also identify the need for studies on other forms of connective tissue disease. Unfortunately, since these are rare diseases, it will be difficult to perform large studies.
Finally, the authors call for studies to compare cyclophosphamide with anti-fibrotic agents or to compare both with placebo, especially in patients with evidence of rapidly progressive fibrotic disease. These studies should aim to determine the optimal treatment duration for induction therapies, as well as the optimal combination and duration of maintenance therapies. The authors suggest that because connective tissue disease-associated ILD is rare, national registries may help researchers identify patients with rare lung diseases who would be eligible for such a clinical trial.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
Fast Facts
- A Cochrane review found no clear evidence that patients treated with cyclophosphamide had better lung function than patients treated with mycophenolate mofetil.
- The authors of the systematic review cautioned that physicians should expect treatment with cyclophosphamide to result only in a modest improvement in the preservation of forced vital capacity.
- Patients treated with cyclophosphamide should be monitored for adverse effects during treatment, as well as in the years following treatment.
References
- Barnes H, Holland AE, Westall GP, et al. Cyclophosphamide for connective tissue disease-associated interstitial lung disease. Cochrane Database Syst Rev. 2018 Jan 3;1:CD010908.
- Tashkin DP, Roth MD, Clements PJ, et al. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomised controlled, double-blind, parallel group trial. Lancet Respir Med. 2016 Sep;4(9):708–719. Epub 2016 Jul 25.
