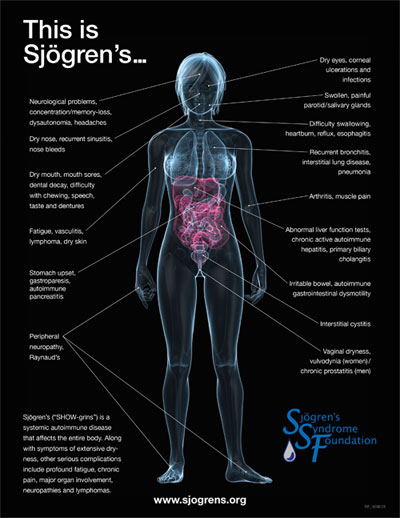
 April is Sjögren’s Awareness Month and the perfect time for rheumatologists to become proactive and learn more about this autoimmune disease, including newly published, evidence-based guidelines. As many as 4 million Americans, mostly women, suffer from Sjögren’s syndrome, and as many as 2.5 million remain undiagnosed, according to the Sjögren’s Syndrome Foundation (SSF).1
April is Sjögren’s Awareness Month and the perfect time for rheumatologists to become proactive and learn more about this autoimmune disease, including newly published, evidence-based guidelines. As many as 4 million Americans, mostly women, suffer from Sjögren’s syndrome, and as many as 2.5 million remain undiagnosed, according to the Sjögren’s Syndrome Foundation (SSF).1
This month, the SSF, which began the awareness campaign in 1998, will use its social media channels (Twitter @SjogrensOrg, Facebook @SjogrensSyndromeFoundation, and LinkedIn Sjögren’s Syndrome Foundation) to educate healthcare professionals and the general public about the disease, highlighting facts and figures, resources and patient testimonials. Key promotions this year include the results of SSF efforts to reduce time to diagnosis, increased interest in Sjögren’s-focused clinical trials and clinical practice guidelines published in the April 2017 issue of Arthritis Care & Research.2
 “It is an exciting time,” says Nancy Carteron, MD, FACR, senior scientific consultant in rheumatology and immunology and clinical associate professor of medicine at the University of California, San Francisco. “I feel there has been a shift in awareness and understanding within a one- to two-year period. The number of people publishing novel research in Sjögren’s syndrome is exponentially increasing. And people are coming from other specialties, including hematology, pulmonology, dermatology … that is a really exciting thing, too. It is going to drive understanding of the disease.”
“It is an exciting time,” says Nancy Carteron, MD, FACR, senior scientific consultant in rheumatology and immunology and clinical associate professor of medicine at the University of California, San Francisco. “I feel there has been a shift in awareness and understanding within a one- to two-year period. The number of people publishing novel research in Sjögren’s syndrome is exponentially increasing. And people are coming from other specialties, including hematology, pulmonology, dermatology … that is a really exciting thing, too. It is going to drive understanding of the disease.”
Many patients who develop Sjögren’s syndrome also suffer from rheumatoid arthritis or lupus, according to the American College of Rheumatology. Treatments target relief of the most bothersome symptoms, such as dry eyes and mouth, as well as preventing infections or dental disease.3
Dr. Carteron, who serves on the SSF Board of Directors and as chair of the SSF’s Medical and Scientific Advisory Board, notes that it wasn’t that long ago that Sjögren’s syndrome was considered a nuisance disease. In the past four years, however, the SSF has put forth a concentrated effort separate from the Awareness Month that has helped reduce the time to Sjögren’s diagnosis to less than three years, down from nearly six years in 2012. The SSF has set a goal to reduce that time to diagnosis for U.S. patients to 2.5 years by the end of 2017, according to CEO Steven Taylor. He says clinicians have looked at the data and “realized how serious [the illness] can become, and how it can lead to major ailments.”4
“Rheumatologists are really our first line of defense in recognizing, diagnosing and properly treating Sjögren’s disease,” he says. “These guidelines give them a roadmap, which they really have not had with Sjögren’s syndrome. I think that has been frustrating to rheumatologists, because some of the cases are complicated, and [rheumatologists] may not always know what to do.”
Dr. Carteron loosely compares the landscape for Sjögren’s syndrome with the rheumatoid arthritis scene before biologic treatments were introduced. She acknowledges clinician frustrations in treating these patients, citing difficulties with insurance and authorizations. But she encourages rheumatologists to be the first responders for this patient population, many of whom go 10, 15, even 20 doctor visits before receiving a proper diagnosis.
“My message to my colleagues is that we are trained as internists first, so we are trained in every organ system. Rheumatologists have always been a subspecialty that is in a position to connect the dots [of symptoms to achieve a diagnosis],” Dr. Carteron said. “For difficult cases like Sjögren’s syndrome, we are in a great position to connect the dots if we are aware of what those dots might be.
“For example, there is data to suggest that maybe men are likely to even not have SSA/Ro antibodies or SSB/La antibodies. I see male patients referred to me with a negative SSA and SSB. They had horrible dry mouth and their teeth were falling out, but the physician told the patient that they could not have Sjögren’s syndrome. Those patients were never referred to a lip biopsy or other evaluation, which could have led to the Sjögren’s diagnosis.”
Dr. Carteron encourages rheumatologists to check out the new treatment guidelines, as well as related ACR and SSF resources.3,5 She says deep dives into research will uncover most underlying autoimmune conditions.
“Rheumatologists may say, ‘I’m not a dentist’ or ‘I’m not an ophthalmologist,’ but they can connect those dots and send patients to a colleague who is very skilled in eye care,” she explains. “Or, if a rheumatologist doesn’t want to do a Schirmer test in their office, refer [patients] to an ophthalmologist who could.”
Richard Quinn is a freelance writer in New Jersey.
References
- Sjögren’s Syndrome Foundation. About Sjögren’s. 2017.
- Carsons SE, Vivino FB, Parke A, et al. Treatment guidelines for rheumatologic manifestations of Sjögren’s syndrome: Use of biologic agents, management of fatigue and inflammatory musculoskeletal pain. Arthritis Care Res (Hoboken). 69(4):517–527. doi: 10.1002/acr.22968.
- American College of Rheumatology. Sjogren’s syndrome. 2017.
- Sjögren’s Syndrome Foundation. Breakthrough goal: SSF launches five-year breakthrough goal. The Moisture Seekers. 2012 Jan 24.
- Sjögren’s Syndrome Foundation. Brochures and resource sheets.
Help SSF Educate Patients, Families, Caregivers
Sjögren’s Awareness Month aims to educate healthcare professionals and the public about the autoimmune disorder that affects 4 million Americans—with as many as 2.5 million still undiagnosed. Via social media, SSF will deliver disease factoids, resources and patient stories throughout the month, as well as encourage participants to use and follow the hashtags #ThisisSjogrens or #SjögrensAwarenessMonth. Join the conversation at:
- Twitter (@SjogrensOrg)
- Facebook (@SjogrensSyndromeFoundation)
- LinkedIn (Sjögren’s Syndrome Foundation)


