ACR Convergence 2024—With poor sleep a major complaint among patients with rheumatologic diseases, physicians should hone their understanding of how the body regulates sleep and how this system can be disrupted, and tailor their management plans to help patients with these issues, panelists said in a session at ACR Convergence.
ACR Convergence 2024—With poor sleep a major complaint among patients with rheumatologic diseases, physicians should hone their understanding of how the body regulates sleep and how this system can be disrupted, and tailor their management plans to help patients with these issues, panelists said in a session at ACR Convergence.
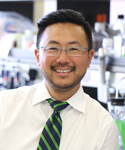
For some patients, their struggles with getting quality sleep couldn’t be more apparent—he has seen patients asleep as he enters the exam room during office visits, said Alfred Kim, MD, PhD, associate professor of rheumatology at Washington University.
“We know our patients are tired because when we walk into the room their eyes are shut and we really have no idea what to do with that,” he said. “The things that bother patients the most are the things we really need to focus our research efforts on. … Sleep is usually the first or second manifestation our patients with lupus complain about.”
How Sleep Works
How the circadian system works to regulate sleep is “misunderstood by rheumatologists,” Dr. Kim said, suggesting that a better appreciation could only help them provide better care.
Light is the main trigger and input for nearly all of the circadian rhythms of the body—prompting melatonin production, lowering body temperature and other changes that promote sleep. In fact, the suprachiasmatic nucleus part of the hypothalamus—which controls the body’s “central circadian rhythm”—has only one input and it’s from the retina. In other words, light, Dr. Kim said.
The body’s circadian rhythms are essentially regulated by the accumulation and degradation of proteins produced by the body’s “clock genes,” including clk, tim, per and bmal1. From there, the peripheral circadian rhythms are dictated by the central circadian rhythms but are additionally influenced by liver activity determined by when we eat, and by exercise, he said.
“‘I’m bringing this up because a leading risk factor for cardiovascular events in humans is discordance between central and peripheral circadian rhythms,” he said. “A leading cause of mortality in our rheumatic disease patients is cardiovascular events.”
Glucocorticoids can reset the body’s peripheral circadian rhythms, so the timing of these medications might be very important, he said. What’s more, he said, sleep is a learned behavior. Therefore, “you can unlearn it,” associating sleep cues with increased attention to pain and actually prompting a drive to avoid sleep, he said.
Correlations with Rheumatic Disease
A study out of Taiwan found that patients with lupus who had non-apnea sleep disorders had an increased risk of acquiring lupus or rheumatoid arthritis.1