What Is Telerheumatology?

Dr. Pearson
Telemedicine means clinical delivery of medical care from a distance—aided and supported through technology.
Prior to the COVID crisis, Medicare coverage of medical visits done via telemedicine was limited to specific circumstances, such as patients living in rural areas. But in March, the Centers for Medicare & Medicaid Services (CMS) issued a set of Medicare 1135 waivers that relaxed restrictions and broadened access to telehealth services and coverage for visits, whether office, hospital or other visits, including over the telephone. These include virtual check-in services between a patient and doctor by audio or video devices, whether a new or established patient, and remote patient monitoring. The waiver also allows previously unapproved communication technologies, such as FaceTime or Skype.
“Medicare beneficiaries across the nation, no matter where they live, will be able to receive a wide range of services via telehealth without ever having to leave home,” CMS Administrator Selma Veera announced during a White House briefing on March 17. How this flexibility is being used by rheumatologists at this time and whether former telemedicine policies will be restored or revised after the crisis is lifted remain unknown.
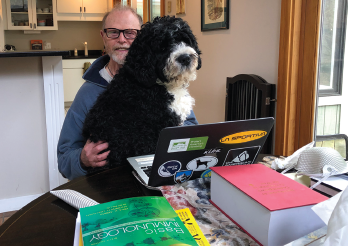
Dr. Albert conducts a telerheumatology with an assist from his “esteemed colleague,” Zeus.
But at this time, the CMS will reimburse synchronous telemedicine visits at the same fee-for-service rate as regular, face-to-face evaluation and management visits, using the regular evaluation and management codes for new patient visits (99201–99205), established patient visits (99212–99215) and consultations (99241–99245). Telephone assessment and management services by all qualified healthcare professionals can be billed for times of 11–20 minutes or 21–30 minutes, using codes 98967 or 98969, respectively. Virtual check-ins and e-visits have their own codes. For more information, see the ACR’s Telehealth Provider Fact Sheet.
The spectrum of healthcare provided with telemedicine is broader than many people realize, says Duane Pearson, MD, of the Rheumatology Clinic, University of Colorado School of Medicine, Aurora. “There are a lot of opportunities to meet patients where they need us, if we can leverage the available modalities and work to dismantle the barriers.”
Telemedicine can be used to diagnose rheumatic conditions, manage disease and provide necessary follow-up. The provider can establish a relationship with the patient and then triage services based on disease severity and complexity. For rheumatologists, conditions to target with telemedicine include osteoporosis, polymyositis, Sjögren’s syndrome, scleroderma, vasculitis and lupus—although lupus can be harder to diagnose remotely.
The program at the University of Colorado has followed the lead of Dartmouth-Hitchcock Medical Center’s Connected Care and Center for TeleHealth, based in Hanover, N.H., which offers rheumatology appointments via telemedicine for evaluations, follow-up exams and recommendations of relevant therapies using live two-way secure video on large-format, high-definition mobile carts. Dartmouth-Hitchcock rheumatologist Daniel Albert, MD, and colleagues mix periodic in-person visits to smaller hospitals with telemedicine.2
“Like any technology, telemedicine has lots of ramifications. The barriers are real, but slowly going away,” Dr. Albert says. “I believe [the use of] telerheumatology will grow.”
The COVID-19 pandemic is accelerating the pace of that change.
Dr. Pearson’s program in Colorado uses a similar model, partnering with rural and safety net hospitals to provide episodic, on-site rheumatology care and telemedicine for ongoing follow-up to clinics up to 300 miles away as part of a pre-appointment consult triage system to identify patients who require timely evaluation and treatment.3 It also participates in Project ECHO, developed in New Mexico, an innovative program that connects community providers with specialists, including rheumatologists, at centers of excellence through real-time video encounters.4 Sessions using case-based learning and mentorship help local healthcare providers gain the expertise needed to provide services and facilitate patient transitions in and out of specialist care.
Some rheumatologists are comfortable providing services remotely via telemedicine, and just as many voice concerns about not seeing their patients in person, Dr. Pearson says. “A hybrid model like ours can address both concerns, and by focusing on the sickest patients who require active ongoing management, it makes more efficient use of scarce specialist resources. By leveraging the full spectrum of tele/remote care, including direct video encounters, e-consults and ECHO, we have the best opportunity to provide rural providers and patients the care they need.”
Research has documented the ability of telemedicine-based encounters to identify rheumatic diagnoses that are later confirmed by in-person visits.5
Dr. Pearson believes lack of coverage by insurers will become less of a drawback as leading managed care plans engage with and pay for telemedicine. Turning back the clock after the pandemic is controlled may prove difficult.
Other barriers are regulatory, such as the challenge of interstate regulations. Dr. Pearson says, “For every hospital we work with, we have to be credentialed, and then recredentialed every two years, although Colorado’s standardized credentialing process makes this less of a burden.”
Editor’s note: Many of these barriers have, at least temporarily, been lifted to ease the medical burden during the COVID-19 pandemic. See the Legal Update column from our April issue and the ACR’s guidance for rheumatologists providing telemedicine during this national emergency.



