The Case
A 56-year-old white woman was evaluated for a one-year history of painless bumps on the dorsal aspect of the proximal interphalangeal (PIP) joints of both hands and suspected flexor tenosynovitis in her palms. On examination, small cystic nodules without erythema or tenderness were present on the dorsal aspect of several PIP joints (see Figure 1). The PIP joints had normal range of motion and no swelling or tenderness. She had induration along the course of the third flexor tendon without frank triggering or contractures. Hand radiographs were normal.
A musculoskeletal ultrasound examination was performed to assess for synovitis and tenosynovitis and to evaluate the nodules on the PIP joints and the palms. The ultrasound demonstrated the underlying third PIP joint and extensor tendon were normal, but it revealed a cystic, semi-lobulated lesion with hypoechoic and isoechoic features, which was partially compressible (see Figures 2 and 3) and exhibited a mild (grade 1) Doppler signal.
An evaluation of the palmar aspect of the right hand revealed an ill-defined hypoechoic lesion superficial to the flexor tendon proximal to the third metacarpophalangeal (MCP) joint (see Figures 4 and 5). It did not move with the underlying tendon, and the lesion had no Doppler signal. The underlying flexor tendon, the MCP joint and the A-1 pulley were normal. Diagnosis of PIP joint knuckle pads, in association with Dupuytren’s contracture, was made. No further intervention was recommended.
Discussion
Knuckle pads are benign subcutaneous nodules on the dorsal aspect of the PIP joints. Rarely, they are seen on the dorsal aspect of the MCP joints.1 These fibro-fatty nodules can be bilateral and are painless. Knuckle pads are usually idiopathic, although rare associations have been reported with repeated trauma and Dupuytren’s contractures.2-4 They are not associated with underlying joint or tendon abnormalities.
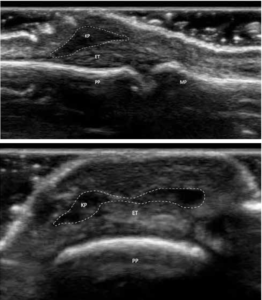
FIGURES 2 & 3: Dorsal longitudinal and transverse B-mode ultrasound views of the knuckle pads. Subcutaneous hypoechoic mass can be seen (enclosed in dotted lines). Key: MC: metacarpal; PP: proximal phalanx; ET: extensor tendon; KP: knuckle pad. (Click to enlarge).
No intervention is needed for these benign nodules. They usually come to the physician’s attention for cosmetic reasons or due to concerns of arthritis. An accurate diagnosis should be made after excluding other causes, such as gouty tophi, rheumatoid nodules, ganglion cysts, Bouchard nodes, synovitis and other rarer causes of nodules, such as multicentric reticulohistiocytosis.
Musculoskeletal ultrasound can be an important tool in confirming the diagnosis of knuckle pads. On gray-mode sonography, knuckle pads are hypoechoic, subcutaneous masses with ill-defined margins that are usually non-compressible.5 Doppler usually does not show any hypervascularity in the nodule, although peripheral hypervascularity has been rarely reported.6 The underlying joint and tendon are usually normal. Histopathology of knuckle pads reveals myofibroblast proliferation and decreased elastic filaments in the dermis. The epidermis and corneum are normal.5
Similar to our case, knuckle pads in association with Dupuytren’s contractures have been reported.2 Dupuytren’s contractures are secondary to fibrous thickening of the palmar fascia, leading to firm palmar nodules and cords. On musculoskeletal ultrasound, these subcutaneous nodules in the palmar fascia are directly superficial to the flexor tendons and appear hypoechoic. Hypervascularity on color Doppler is usually absent and the lesions are non-compressible. Typically, the length of these lesions is greater than the width.7
In contrast, flexor tenosynovitis of the flexor tendons of the hands appears as a hypoechoic or anechoic compressible swelling around the tendon (i.e., visible both above and beyond the tendon) with increased color Doppler signal and is accompanied by thickening and loss of the normal fibrillar pattern of the tendon.8
Gouty tophi can also appear on the dorsal, as well as the volar, aspect of the PIP joints. They are usually soft to firm and non-tender. Sonographically, they are heterogeneous and can be multilobulated.9 They can contain hyperechoic calcifications with acoustic shadowing.10 The underlying joint may reveal a double contour sign secondary to crystalline deposition on the cartilage surface.11 Juxta-articular erosions may also be seen underneath the tophaceous deposits.9,12 Hypervascularity can be seen around the periphery of the tophus.
Rheumatoid nodules are also painless, soft to firm, non-tender nodules and can appear on the dorsal or volar aspect of the PIP joints. Sonographically, they are homogenous hypoechoic nodules with hyperechoic rims and may have anechoic centers.10 Features of synovitis, such as synovial hypertrophy, effusion and hypervascularity with increased color Doppler uptake, may be present. In addition, periarticular erosions can also be seen, although the nodules themselves are less erosive to the bone, and cortical bone is easily seen underneath the nodule.10
Synovitis of the PIP joints can also mimic knuckle pads. In contrast to knuckle pads, synovitis is associated with pain, tenderness and limited mobility of the PIP joint. Ultrasound reveals effusion, synovial hypertrophy and increased color Doppler signal in the PIP joint.
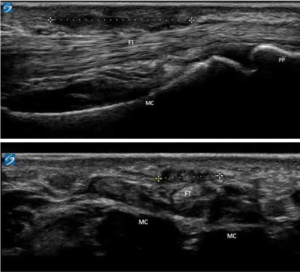
FIGURES 4 & 5: Palmar longitudinal and transverse B-mode ultrasound views of the Dupuytren’s contracture. An ill-defined hypoechoic lesion superficial to the flexor tendon proximal to the metacarpophalangeal joint can be seen (dotted line). Key: MC: metacarpal; PP: proximal phalanx; MP: Middle phalanx; FT: flexor tendon. (Click to enlarge.)
Ganglion cysts are usually soft, non-tender cystic to firm swellings and can be present, rarely, on the dorsal aspect of the PIP joints. On musculoskeletal ultrasound, they are anechoic to hypoechoic with increased posterior acoustic enhancement.13 Ganglion cysts are usually seen in proximity to underlying tendons and can originate from the tenosynovium of the tendon. Power Doppler does not usually reveal hypervascularity, and the joint underneath is normal.10
Bouchard nodes are firm to hard, non-tender nodules seen on the dorsal aspect of the PIP joints in osteoarthritis. Ultrasound usually reveals underlying osteophytes and can reveal joint effusion. Erosions can be detected by musculoskeletal ultrasound in erosive osteoarthritis.14
In Sum
Knuckle pads are benign, subcutaneous, soft-tissue nodules. Musculoskeletal ultrasound can be a useful tool in diagnosing knuckle pads and ruling out other etiologies.
Pankaj Bansal, MD, RhMSUS, serves in the Department of Rheumatology, Mayo Clinic Health System, Eau Claire, Wis.
Eugene Kissin, MD, RhMSUS, is a clinical professor in the Division of Rheumatology, Boston University School of Medicine.
Fawad Aslam, MBBS, RhMSUS, RMSK, is a rheumatologist at the Mayo Clinic in Scottsdale, Ariz.
References
- Nenoff P, Woitek G. Images in clinical medicine. Knuckle pads. N Engl J Med. 2011 Jun 23;364(25):2451.
- Mikkelsen OA. Knuckle pads in Dupuytren’s disease. Hand. 1977 Oct;9(3):301–305.
- Dickens R, Adams BB, Mutasim DF. Sportsrelated pads. Int J Dermatol. 2002 May;41(5):291–293.
- Rayan GM, Ali M, Orozco J. Dorsal pads versus nodules in normal population and Dupuytren’s disease patients. J Hand Surg. 2010 Oct;35(10):1571–1579.
- Tamborrini G, Gengenbacher M, Bianchi S. Knuckle pads—A rare finding. J Ultrason. 2012 Dec;12(51):493–498.\
- Lopez-Ben R, Dehghanpisheh K, Chatham WW, et al. Ultrasound appearance of knuckle pads. Skeletal Radiol. 2006 Nov;35(11):823–827.
- Morris G, Jacobson JA, Kalume Brigido M, et al. Ultrasound features of palmar fibromatosis or Dupuytren contracture. J Ultrasound Med. 2019 Feb;38(2):387–392.
- Hmamouchi I, Bahiri R, Srifi N, et al. A comparison of ultrasound and clinical examination in the detection of flexor tenosynovitis in early arthritis. BMC Musculoskelet Disord. 2011 May 8;12:91.
- Thiele RG, Schlesinger N. Diagnosis of gout by ultrasound. Rheumatology (Oxford). 2007 Jul;46(7):1116–1121.
- Nalbant S, Corominas H, Hsu B, et al. Ultrasonography for assessment of subcutaneous nodules. J Rheumatol. 2003 Jun;30(6):1191–1195.
- Ogdie A, Taylor WJ, Neogi T, et al. Performance of ultrasound in the diagnosis of gout in a multicenter study: Comparison with monosodium urate monohydrate crystal analysis as the gold standard. Arthritis Rheumatol. 2017 Feb;69(2):429–438.
- Ottaviani S, Bardin T, Richette P. Usefulness of ultrasonography for gout. Joint Bone Spine. 2012 Oct;79(5):441–445.
- Stacy GS, Bonham J, Chang A, Thomas S. Soft-tissue tumors of the hand—imaging features. Can Assoc Radiol J. 2020 May;71(2):161–73.
- Wittoek R, Jans L, Lambrecht V, et al. Reliability and construct validity of ultrasonography of soft tissue and destructive changes in erosive osteoarthritis of the interphalangeal finger joints: A comparison with MRI. Ann Rheum Dis. 2011 Feb;70(2):278–283.




