Although reporting for Stage 1 of the Centers for Medicare and Medicaid Services (CMS) Electronic Health Record (EHR) Incentive Program began just this year, the rules, objectives, and measures for Stage 2 are already being established. Last June, the Office of the National Coordinator (ONC) for Health Information Technology (IT) presented CMS with its recommendations for Stage 2 of the CMS EHR Incentive Program which builds on the Stage 1 objectives supporting EHR utilization for data capture and sharing.
The CMS EHR Incentive Program offers incentive payments of up to $44,000 for eligible providers, including rheumatologists who successfully demonstrate meaningful use of their EHR system, meeting the program’s measure thresholds for established objectives. Under the provisions of the Health Information Technology for Economic and Clinical Health Act (HITECH), CMS estimates that between $14.1 and $27.5 billion in funding will be distributed through the EHR Meaningful Use incentive program.
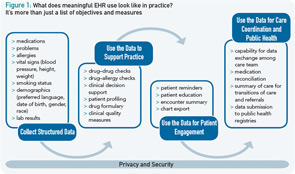
This incentive program is meant to not only lend support for the acquisition of EHR systems, but also to ensure that systems purchased are capable of meeting the minimum requirements for secondary utilization and exchange of health information. As the name implies, the incentive program focuses on how EHR systems are used in practice, rather than simply providing incentives for their purchase. The requirements for the program are meant to encourage providers to use the system as more than simply an electronic medical chart; by letting go of “paper thinking,” providers can begin to realize the potential for an electronically supported practice transformation leading to greater efficiency, improved quality, and effectively coordinated care.
As with Stage 1 objectives, the Stage 2 program should not be viewed as a list of unique items and thresholds to meet, but as building blocks to further drive advanced utilization of the EHR system for disease management, clinical decision support, medication management, support for patients’ access to their health information, quality measurement and research, and bidirectional communication of health data (see Figure 1).
Potential Stage 2 Objectives and Measures
Many of the proposed objectives and measures for Stage 2 of the CMS EHR Incentive Program have been carried over from Stage 1 of the program, with some adjustments to the measurement thresholds and with the designation of “core” or required objective applied to those that were “menu” or optional in Stage 1 (see Table 1). For most, this will mean that your practice will simply need to evaluate practice workflows to ensure that the entire practice team has an understanding of who is responsible for the clinical and administrative actions and that these actions are being done in a way that is consistent with measurement in the EHR system.
New requirements for providers might include collecting structured data that document patient communication preferences, listing the care members for patients, recording the availability of an advanced directive for patients over 65, and the use of electronic patient communication tools like secure messaging.
Continued below…
Table 1: Objectives
Unchanged objectives
- Maintain medication list (80%)
- Maintain problem list (80%)
- Maintain allergy list (80%)
Objectives moved from menu to core
- Incorporate lab results as structured data (40%, use LOINC where available)
- Implement drug-formulary checking (internal or external)
- Medication reconciliation (50%)
Objectives moved from test to routine and core
- Submit immunization data (at least once)
- Submit reportable lab results (at least two)
- Submit syndromic surveillance date (eligible hospitals, consider for eligible professionals [EP]) (at least once)
Objectives with threshold changes (now all core measures)
- CPOE for >60% of Meds and Lab, Radiology CPOE in use
- E-prescribing for 50% of outpatient prescriptions
- 80% of patients have demographics recorded with more granular categories
- 80% of patients 3 years old and over have vital signs during reporting year
- 80% of patients over 13 years old have smoking status recorded
- 10% of active patients are sent reminders (beyond appointments) (EP)
- 50% of transitions in care have summary of care record provided and 10% of discharges, and 25 EP transactions include a plan of care and provider list, transmit the information electronically
- 10% of patients access health information electronically (EP)
- 50% provided a visit summary within 24 hours online access available
- 10% of all patients receive patient-specifi c educational materials
- Generate patient lists for multiple patient-specifi c parameters
New objectives for Stage 2
- Hospitals send 40% of clinical lab results to outpatient providers as structured data (when electronic order), LOINC if available
- E-Prescriptions for 20% of discharge medications (hospitals)
- 30% of visits have searchable electronic EP note
- 30% of hospital days have one searchable electronic note by physician, PA, or NP
- Electronic medication administration in at least one hospital unit (with electronic “5 Rights” checking)
- 10% of patients/families have ability to access and download information about hospital stay
- 25 patients have sent secure messages (EP)
- 20% of patients have communication preferences recorded
- 10% of patients have list of care team members available electronically
- 50% of hospital patients and 25 patients of an EP over 65 years old, have electronic record of whether advanced directive exists and if exists can access that advanced directive
Proposed Schedule Changes
The ONC has also recommended schedule changes for the EHR Incentive Program that will affect those providers who began attestation in 2011. The original program schedule, which had Stage 2 attestation scheduled to begin in 2013 for those who attest in 2011, imposed an accelerated timeline (approximately one year) on EHR vendors to develop supporting functionality and certify for Stage 2, then install these upgrades in practices. Taking into consideration this timeline—deemed unreasonable by many—the ONC is proposing to relax the schedule. This eliminates the “penalty” for early adopters and allows organizations that start in 2011 to get three years of incentive payments under Stage 1. Those beginning attestation for Stage 1 in 2012 will continue on the established schedule, submitting for Stage 1 in 2012 and 2013, then begin Stage 2 attestation in 2014. This revised timeline should relieve some of the pressure and give providers more time to install upgrades prior to the beginning of the Stage 2 reporting period, increasing the likelihood of successfully achieving meaningful use and collecting incentive payments in that reporting year.
It’s About Better Care
With the availability of substantial incentive funds and evolving program requirements, it’s easy to lose sight of the big picture and the overall goals of the meaningful utilization of health IT in clinical practice. EHR systems should be implemented in practice not just as a means to meet program requirements, but as a vehicle to deliver better care. Meaningful utilization of health IT is about the creation of an electronically enabled environment that supports the collection and use of meaningful information about unique patients that can provide a complete picture of their health and how their disease is affecting their everyday life—and which can be used as a tool to support the patient as an active member of his or her healthcare team.
For more information on criteria for participation and successful reporting for the CMS EHR Incentive Program, please visit www.rheumatology.org/HIT or contact Itara Barnes in the ACR’s Quality and Health Informatics department at [email protected].